
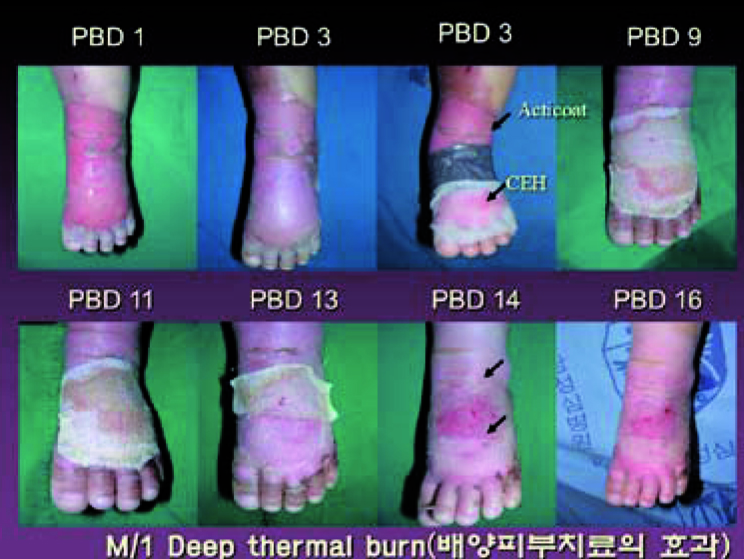

Figure 1. Biologic dressing using cultured keratinocytes
Biologic Dressing with Collagen
Collagen is abundantly found in most vertebrates. It mainly provides structural support to living tissues but at the cellular level, it also promotes cellular adhesion, migration and supports cellular growth. As collagen plays many important roles in various stages of wound healing, it has long been regarded as an important substance in wound healing.
In Korea, collagen products with varying sizes and thicknesses are available and have excellent efficacy in deep second degree and third degree burns.
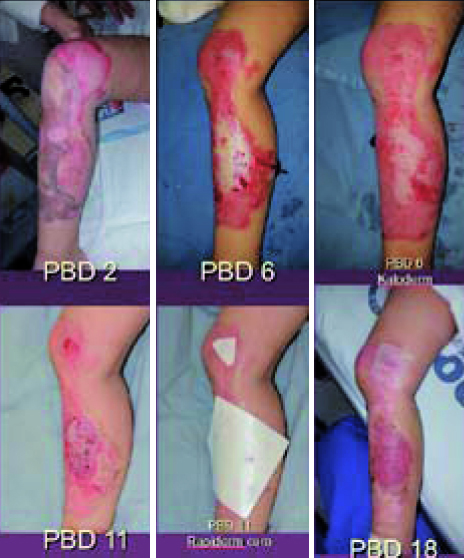
Figure 2. Biologic dressing using collagen.
Biologic Dressing Using Amnion
Amnion dressing is a type of allogeneic skin flap. Unlike the xenograft, allograft effectively removes bacteria and promotes active vascularization. Despite such efficiency, however, there were serious difficulties including scarcity of the donor, problems with storage, and the risk of vertical transmission, etc. Dried bovine amniotic membrane improves upon such limitations and has major advantages such as accelerated epithelization, reduced scarring and pigmentation, and convenience of use.

Figure 3. Biologic dressing using amnion.
Biologic Dressing Using Growth Factors
As more is known about the role of growth factors in wound healing, growth factors are being widely used in wound healing. Basic fibroblast growth factors (bFGFs) promote proliferation of fibroblasts, vascularization, and formation of granulation tissues. Genetically recombined bFGFs were commercialized in the form of a spray, which can help reduce the ulcer size, shorten treatment, and accelerate reepithelization.
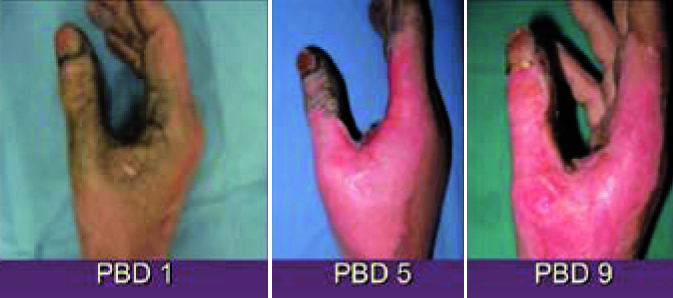
Figure 4. Biologic dressing using growth factors
Change in Patients’ Expectations; from ‘Survival’ to ‘Quality of Survival’
Thanks to marked improvements in the medical technology in treating infection, shock, and gastroenterological dysfunctions etc., burn-related mortality has fallen drastically. Recently, the goal of treatment for patients who have survived massive burns is shifting from survival to quality to survival.12,13 More patients are concerned about aesthetic outcomes of treatment as well. This is driving up the demand of high quality wound dressings that can reduce scarring. Development of various biologic dressings reflects such increased demand.
[Advertisement] MAGNUM(Q-switched Nd:YAG Laser) – Manufacturer: (www.i-dana.com)]
Change in Lifestyles
Low socioeconomic status is an important risk factor of burn wounds. Cramped living spaces that are associated with low socioeconomic status raise the risk of burns. Before the gas stoves become commonplace, poor people used a fireplace or furnace to cook food. And the risk of sustaining burns increases drastically with such lifestyles. Currently, the GDP of South Korea is about USD 25,000. With improved economy, we are experiencing better living standards and work environment. This led to a lower incidence of extensive or deep third degree burns. Eschar tissues are characteristic of severe burns of at least third degree. As we see less severe burns with eschar tissues, the use of Silvadine, which is specialized for eschar tissues, is decreasing. Moreover, the development and wide use of moist wound dressing and biologic dressing have slowly phased out Silvadine and gauze in the field of wound care.
References
1. Winter GD. Formation of scab and the rate of epithelialization of superficial wounds in the skin of the young domestic pig. Nature 1962;193:293–4.
2. Hinman CD, Maibach HI. Effect of air exposure and occlusion on experimental human skin wounds. Nature 1963;200:377–8.
3. Robson MC, Krizek TJ. The effect of human amniotic membranes on the bacterial population of the infected rat. Ann Surg 1973;177:144Y149
4. Rheinwald JG, Green H. Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell 1975;6: 331–43.
5. O’Connor NE, Mulliken JB, Banks-Schlegel A, et al. Grafting of burns with cultured epithelium prepared from autologous epidermal cells. Lancet 1981;1:75–8.
6. Hefton JM, Amberson JB, Biozes DG, et al. Loss of HLA-DR expression by human epidermal cells after growth in culture. J Invest Dermatol 1984;83:48–50.
7. Thivolet J, Faure M, Demidem A, et al. Long-term survival and immunological tolerance of human epidermal allografts produced in culture. Transplantation 1986;42:274–80.
8. Thivolet J, Faure M, Demidem A, et al. Cultured human epidermal allografts are not rejected for a long period. Arch Dermatol Res 1986;278:252–4.
9. McGuire J, Birchall N, Cuono C, et al. Successful engraftment of allogeneic keratinocyte cultures in recessive dystrophic epidermolysis bullosa. Clin Res 1987;35:702A.
10. De Luca M, Albanese E, Cancedda R, et al. Treatment of leg ulcers with cryopreserved
allogeneic cultured epithelium: a multicenter study. Arch Dermatol 1992;128:633–8.
11. Teepe RGC, Roseeuw DI, Hermans J, et al. Randomized trial comparing cryopreserved cultured epidermal allografts with hydrocolloid dressings in healing chronic venous ulcers. J Am Acad Dermatol 1993;29:982–8.
12. Brusselaers N, Pirayesh A, Hoeksema H, Richters CD, Verbelen J, Beele H, Blot SI, Monstrey S. Skin replacement in burn wounds. J Trauma 2010;68:490–501.
13. Kamolz LP. Burns: learning from the past in order to be fit for the future. Crit Care 2010;14:106.
14. Markéta Límová, Active Wound Coverings: Bioengineered Skin and Dermal Substitutes; 1237-1255
15. Mathangi Ramakrishnan K., Babu M., Mathivanan, Jayaraman V., Shankar J, Advantages of clooagenbased biological dressings in the management of superficial and superfiacl partial thickness burns in children, Annals of Burns and Fire Disasters – vol. 26; n. 2; June 2013; 98-104
16. Edward Lineen, MD, Nicholas Namias, MD, MBA, FACS, FCCM, Biologic Dressing in Burns, THE JOURNAL OF CRANIOFACIAL SURGERY, vol.19, n. 4 July 2008; 923-928
17. Liesbeth Lootens, Nele Brusselaers, Hilde Beele4 & Stan Monstrey, Keratinocytes in the treatment of severe burn injury: an update, International Wound Journal, 2012; 6-12
-To be continued




















