▶ Previous Artlcle : #4-1. Etiology and Incidence of Varicose Veins
Symptoms
Blood regurgitation caused by valve insufficiency leads to varicose veins symptoms that vary across patients. The venous pressure rises in a standing position and worsens the symptoms. Most patients with varicose veins complain of aesthetic problems caused by dilated vessels, pain, numbness and paresthesia, lower limb fatigue, and edema. They may also experience heaviness of the limbs, tense and tingly muscles, burning and throbbing sensation at the sites of varicose veins. Edema which often occurs when getting out of bed in the morning or standing for a long time without moving lower limbs is especially severe in the foot and ankle and worsens in the evening. Edema disappears or improves after rest. Jakobsen reported that aesthetic problems (79.5%), and fatigue (70.3%) were the most common complaints. Korean reports have also listed aesthetic problem (82%), pain (66%), edema (45%), and heaviness (23%), etc. as the most common complaints.
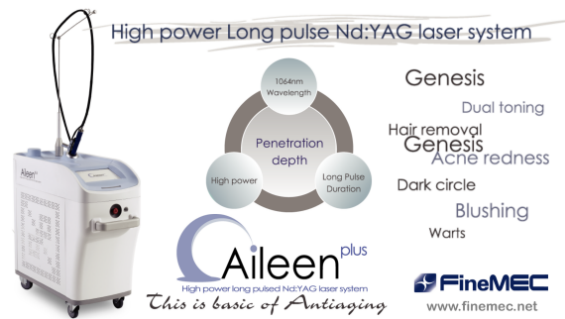
[Advertisement] ▶ Aileen plus(Long pulsed Nd:YAG Laser) – Manufacturer: FineMEC(www.finemec.net)
The results of my study are as following.
Symptoms of varicose veins included aesthetic problem, pain, lower limb edema, lower limb heaviness and fatigue, etc. Symptoms such as pruritus, dermatitis and ulcer were rare. Chief complaints were aesthetic problems in 90% and paresthesia or stiffness in 49% of the patients. This type of pain may arise from dilated veins compressing the dense subcutaneous neural network or lactic acid released by stagnant venous blood. Edema was reported in 10% of patient followed by night cramp in 8%, and dermatitis from venous stasis in 2%. Cases of skin discoloration, skin ulcer, bleeding, superficial thrombophlebitis were also observed.
Thicker and more severe varicose veins were associated with greater frequency of lower limb fatigue and heaviness. However, the severity of varicose veins was not always in direct proportion with symptoms reported by patients. Patients with telangiectasia of 1mm thickness also complained of pain, burning, and fatigue, etc.
Complications
Without treatment, symptoms of varicose veins gradually worsen. Especially, easy bruising, superficial thrombophlebitis, skin discoloration and ulcer etc. may persist. Minor trauma can easily cause bleeding as protruding veins weaken the skin’s protective barrier and the vessel walls of varicose veins become brittle.
Thrombophlebitis: Except for in severe embolism, thrombophlebitis is most commonly caused by varicose veins. An article by a specialist who have treated over 20,000 patients with varicose veins reported that thrombophlebitis develops in about 20% of patients with severe varicose veins. The prevalence in the US was reported to be 0.4% in patients in their 40s, and 1.7% in 70s. Thrombophlebitis is mainly caused by traumatic damage of varicose veins, stasis, and obstruction. Clinical presentations include redness, pain and edema along the course of the veins. In palpation, the veins are hard and tense as tightly pulled strings and pressure pain is felt. The risk of deep vein thrombosis is 9 times higher in patients with thrombophlebitis compared to the general population. Therefore, it is necessary to screen for deep vein thrombosis in patients with thrombophlebitis. Common dermatologic presentations of thrombophlebitis include eczema, dermatitis, and ulcer which are caused by abnormal metabolism between blood vessels and surrounding tissues due to disturbed circulation.
Eczema: varicose eczema have varying presentations; localized type affecting the course of varicose veins, affecting the periphery of ulcer, and spreading to all directions.
Dermatitis: chronic varicose veins is likely to accompany two types of dermatitis; atrophie blanche and venous stasis dermatitis. Atrophie blanche is characterized by smooth and indented vase-shaped white spots appearing in the lower limbs. In most cases, hyperpigmentation around these white spots or talengiectasia are accompanied. Histological presentations show many capillaries connected to the atrophied vessels in center of the lesion. However, this phenomenon cannot be considered as a representative sign of varicose veins. Atrophie blanche also accompanies atherosclerosis, tuberculosis, diabetes, and stasis dermatitis.
Stasis dermatitis is caused by malnutrition in lower limb with circulatory disturbance. It is especially prevalent in obese, middle-aged men and women and is often accompanied by thrombophlebitis or deep vein thrombosis. It often affects the lateral foot which is more susceptible to injury. Lower limb dermatitis can be classified into acute, subacute and chronic types;
① The acute form is caused by trauma, surgery, heat exposure, or underlying disease. It involves painful inflammatory changes.
② The subacute form is characterized by cirrhotic response, red spots, edema, and pain. It is not infectious. It may progress into a chronic form over time or cause functional disturbance.
③ The chronic form results from cirrhosis and ⓐ lower limb dermatitis with cirrhosis and atrophy ⓑ hyperplastic lower limb dermatitis with cirrhosis. Hyperplastic cirrhosis may cause motor disturbance in tibia and tarsal bone by cirrhotic obstruction of the skin. Sign of Gougerot refers to severely hardened, gaiter-shaped hyperplastic changes of the skin that wraps around the lower leg and foot. Skin cirrhosis blocks the circulation of the lymph and causes lymphatic edema. This in turn induces development of ulcer or interferes with the treatment of existing ulcer and exacerbate oxygen deficiency of tissues.
Progression rate
Varicose veins arise from venous valve insufficiency. However, valve insufficiency worsens over time and based on statistics from my practice, patients spend an average 14.4 years from discovery of varicose veins until treatment. As varicose veins is often asymptomatic and left untreated, it leads to many complications mentioned above.
I believe GSV has faster progression than SSV because GSV experiences more pressure due to gravity.
I have arbitrarily named the phase of venous valve anomaly before visible protrusions appear as ‘incubating varicose veins’. This latent period is suspected to last about 3 years in the GSV and 5 years in SSV. However, no studies have investigated this yet.
-To be continued-