▶ Previous Artlcle : #1-1. Anatomic Study of Skin Surface I
B. Superficial Musculoaponeurotic System
Superficial Musculoaponeurotic System (SMAS) is the muscle fibers that surround the facial muscles. SMAS is crucial to understanding the fascia of the face. The facial muscles have important functions of facial expression, mastication and protection of essential organs. They are controlled by facial nerves. Unlike the limb muscles that attach to the bone, facial expression muscles attach to the skin and mucles. Due to this unique structure, facial muscles are able to create various expressions. To carry out these functions normally, a system is needed to harmonize the facial musculature. SMAS has evolved to carry this function. It was first mentioned by Tessier in 1974 and detailed anatomical description was established by Mitz and Peyronie. SMAS divides the subcutaneous fat into two layers. The fibrous septum of SMAS runs across the fat to attach to the dermis. Therefore, SMAS serves as a medium that delivers the facial muscle contraction to the skin (Figure 4).
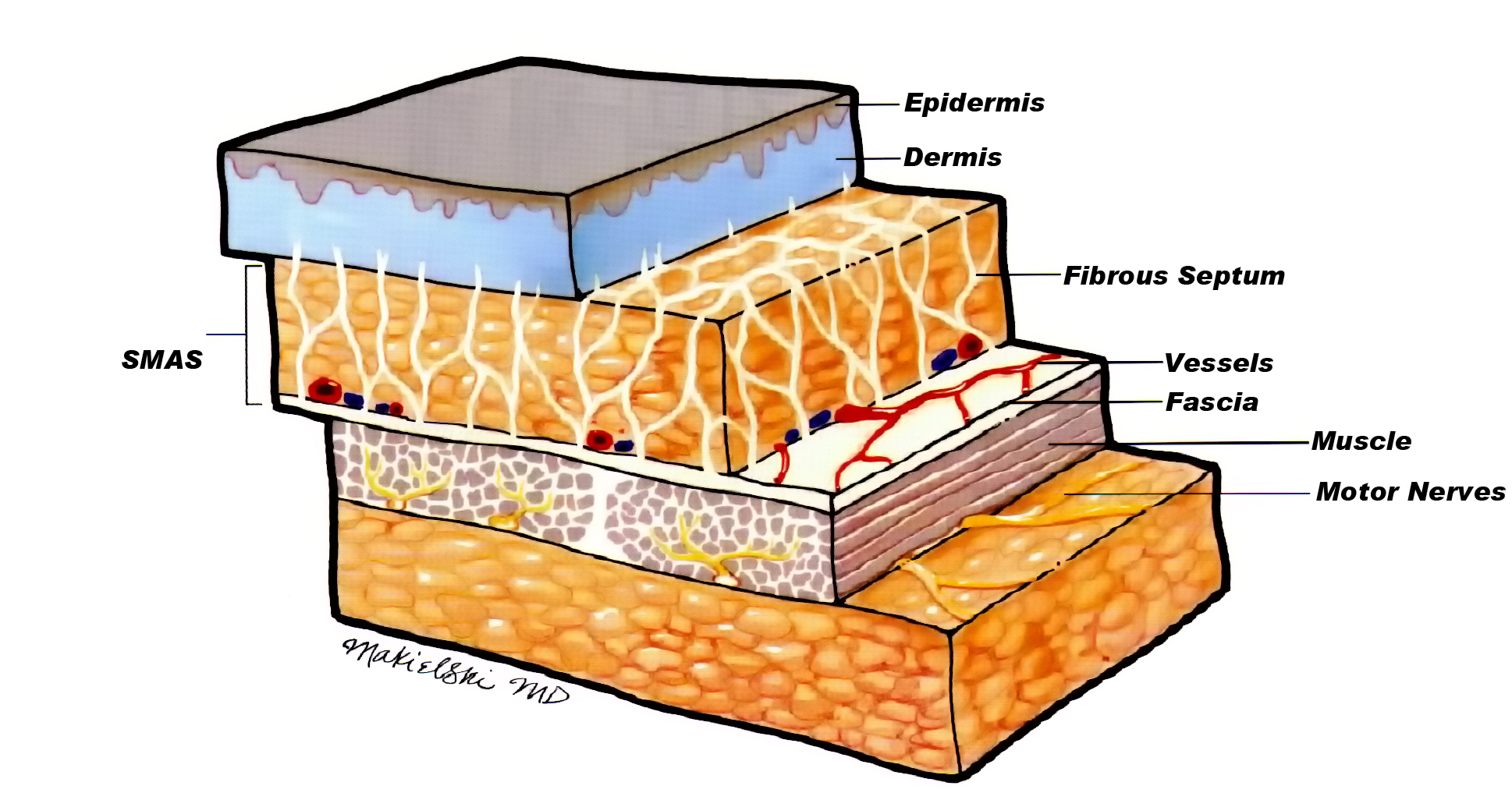
Figure 4 . Cross-section of lower face SMAS.
SMAS is classified into two types; fibrous band that stretches from fascia or periosteum to upper dermis and connection with deep fascia. The fibrous band is again divided into Fasciocutaneous ligament and osteocutaneous ligament based on the site of attachment.
[Advertisement] FCR® (Fractional Prickle CoralCalcium Regentron) – Manufacturer: (www.thermoceutical.asia)]
The former connects the fascia and skin and varies in strength depending on the locality. The Fasciocutaneous ligament is stronger in the scalp, forehead, eye, nose, lip, and chin, whereas it is very loose in the medial cheek or temple. The osteocutaneous ligament lies between the zygoma and lateral chin and provides support to the two structures. SMAS consists of 1-3 muscle fiber layers and its composition varies depending on the location. The deep fascia stretching from the parietal region to the neck needs to encompass various muscles for facial movement and divided and joined together to mimic the functions of galea, frontalis/occipitalis fascia, superfical temporal fascia and cervical superfical fascia (Figure 5).
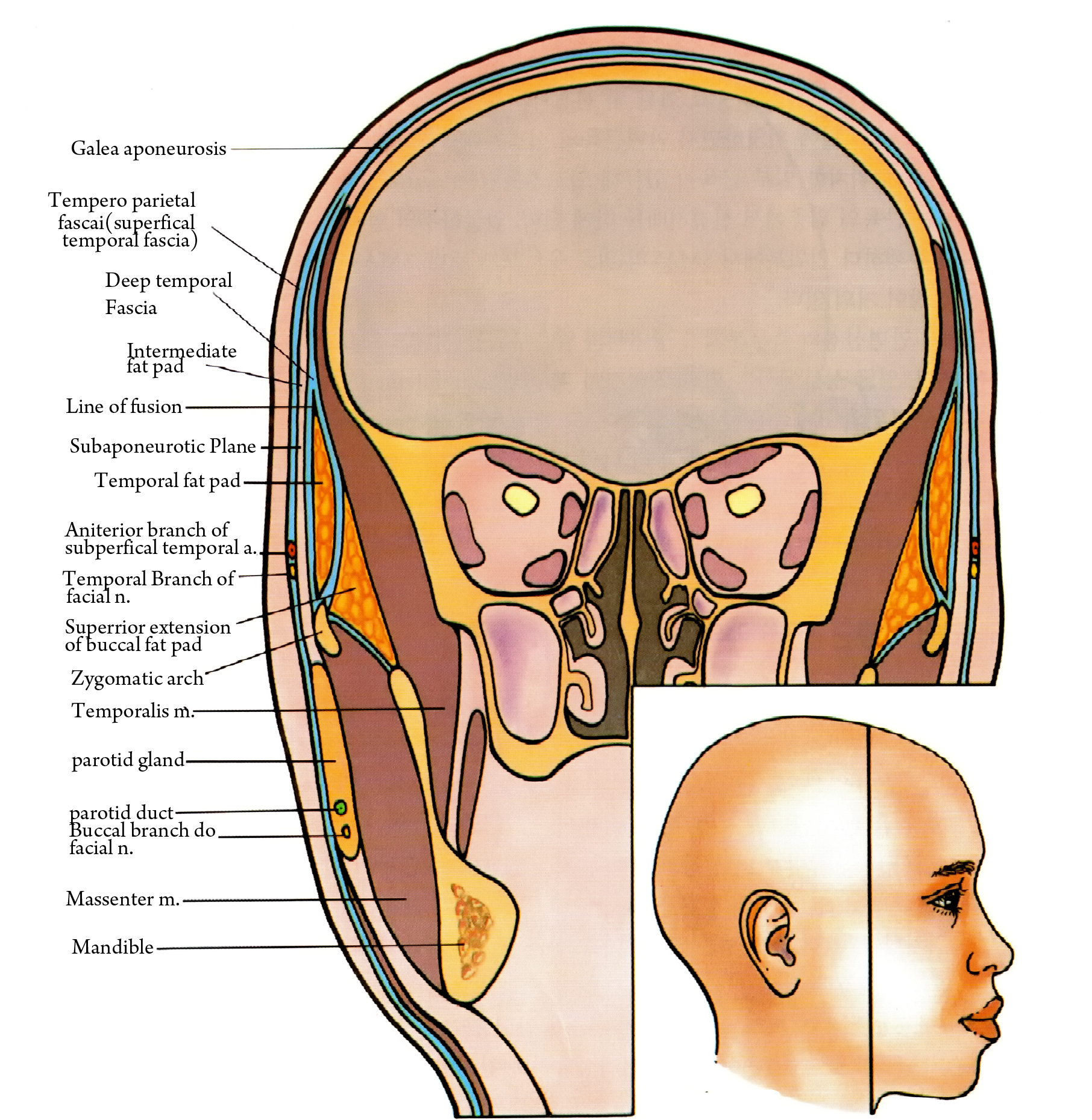
Figure 5. SMAS of face.
The SMAS has better continuity and strength in posterior face whereas it is weaker anterior to nasolabial fold, although the degree varies with age. The SMAS in the temple and zygomatic arch shows discontinuous structure due to connection to fascia, which increases the risk of facial nerve damage. However, based on my clinical experience and cadaver dissection, tissue damage is unlikely when dissection is carried out above the SMAS.
(Table 1) shows the connection of the SMAS to other soft tissues in the face. The SMAS is important to dermatological surgery in two ways besides harmonizing the facial muscles. The relationship between SMAS and other structures is important; the SMAS protects the facial nerves and arteries that lie under or inside it.
Second, it is important for surgical outcome; the fascial layers sag due to aging and create deep lines. The SMAS has to be pulled or repositioned in the classic facelift, thread lift, endotine and aculift, etc. for successful outcome.
C. Facial Nerve
The facial nerve carries the motor nerve function of the facial expression muscles. It originates from stylomastoid foramen, passes posterior to mastoid process and the parotid gland and divides into five branches resembling an open hand. I had a closer look at the facial nerve in a cadaver study and would like to share my experience in this article (Figure 6).
The most superior temporal branch has three branches (Figure 7). First, the upper branch runs straight upward and enters the side of the frontalis muscle. Second, the lower branch stretches in the lateral direction and the middle branch rises. This branch runs toward the lateral canthus and enters the upper orbicularis oculi muscle at the lateral orbital rim. Third, the middle branch passes the outer end of the eyebrow and runs above the orbicularis oculi muscle to enter the corrugator. This course may cause motor impairment when the nerve is damaged. However, dissection following insertion of the guide cannula of AccuSculpt showed that it was stably positioned in the dermis and subcutaneous fat (Figure 8). In the clinical settings, the operation takes place above the SMAS and the risk of damage is quite low. This nerve course can be used in treatment of corrugator impairment and globella wrinkles.
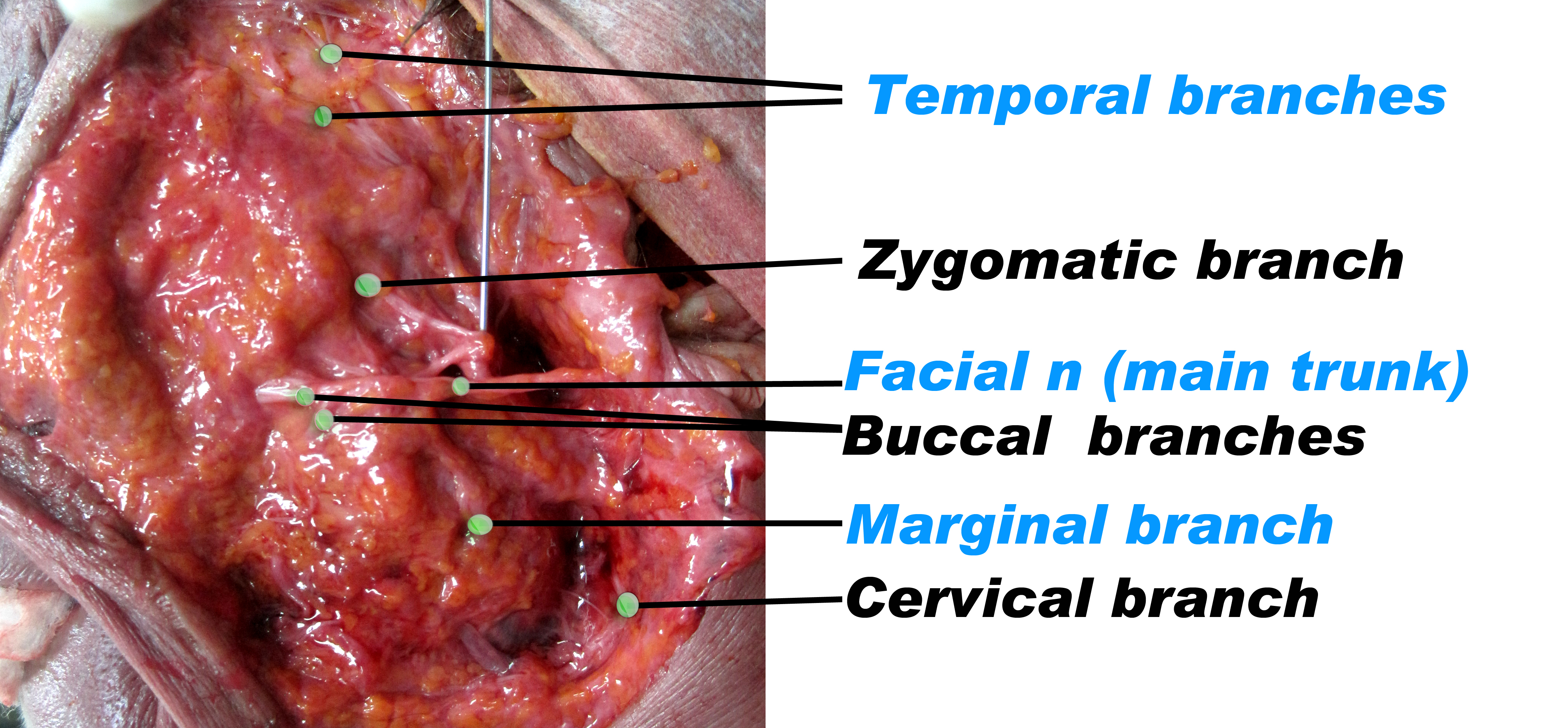
Figure 6.
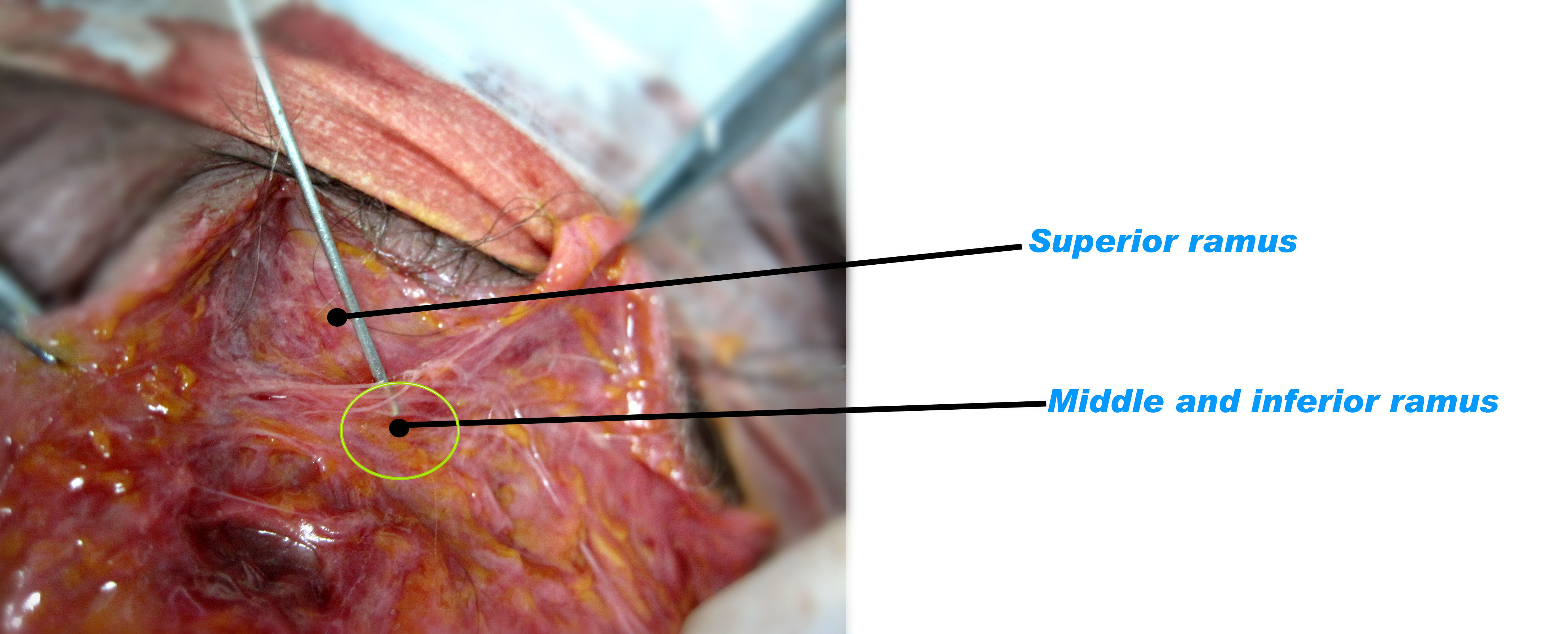
Figure 7. Temporal branch.
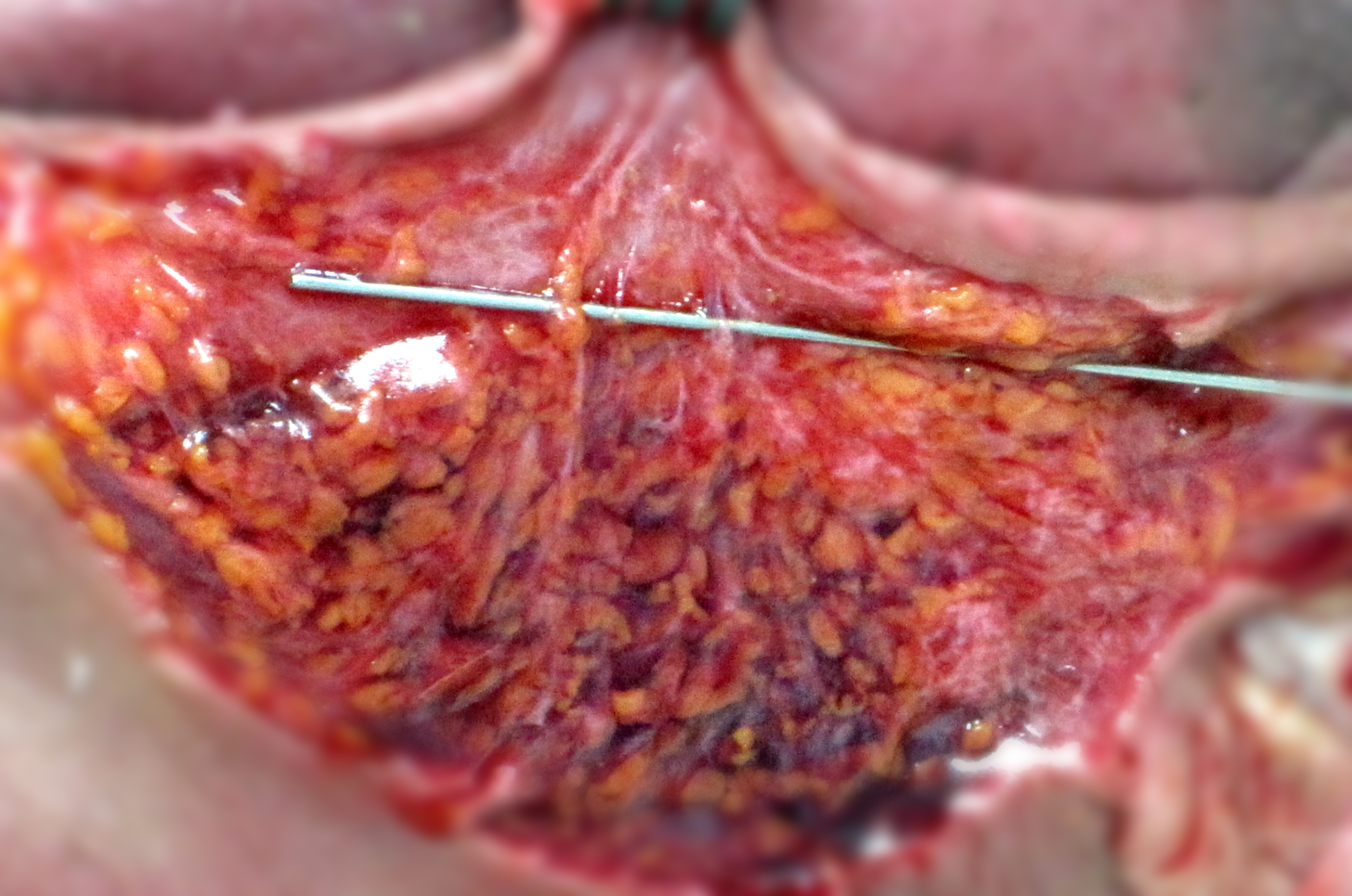
Figure 8. Dissection after cannula insertion. Located in the dermis and subcutaneous fat, safe from infliciting nerve damage.
-To be continued-
▶ Next Artlcle : #1-3. Anatomic Study of Skin Surface I





















