In the past, subciliary incision often carried out in lower eyelid surgery was considered to cause pretarsal flattening. The zygomatic branch of the OOM’s motor nerve was thought to be damaged by incision and tranconjunctival approach was thought to prevent this side effect. However, recent studies reported that the medial side of OOM is more innervated by the buccal branch rather than zygomatic branch. Considering motor nerves pass below the OOM and ascend vertically, subciliary incision alone is not likely to cause pretarsal flattening. Comparative studies have also shown that subciliary incision does not cause pretarsal flattening.
Various methods have been used to create pretarsal fullness from filler injection, fat graft, to tarsal fixation, muscle duplication, dermal substitute, and even insertion of rolled fascia graft. When considering only non-invasive methods, I recommend filler injection as it is difficult to create a thin pretarsal fullness and maintain initial shape long-term with fat graft.
Injection should not be below the inferior palpebral sulcus (where incision is made in lower eyelid surgery) and the needle should be inserted as close to cillia as possible (Image 3). One can feel resistance of soft tissues when injecting in areas adjacent to cillia. The filler should be injected immediately below the point of no resistance. As post-injection massage can send the filler to lower, less resistant area, it is advisable to inject as high as possible.
In patients with dark, thin skin and low likelihood of tyndall effect (translucence), a subcutaneous lever can be used to even out the filler. However, tyndall effect is difficult to predict and shallow injection can cause visible lumps. Therefore, the filler should be injected into the OOM, safely below the skin surface. The degree of tyndall effect is determined by the light wavelength and presence of barrier. When the light wavelength cannot be changed, and in patients prone to side effects, slightly deeper injection increases the amount of barrier and bring better outcome.
In the next article, we will take a look at the midface, particularly, nasolabial folds.
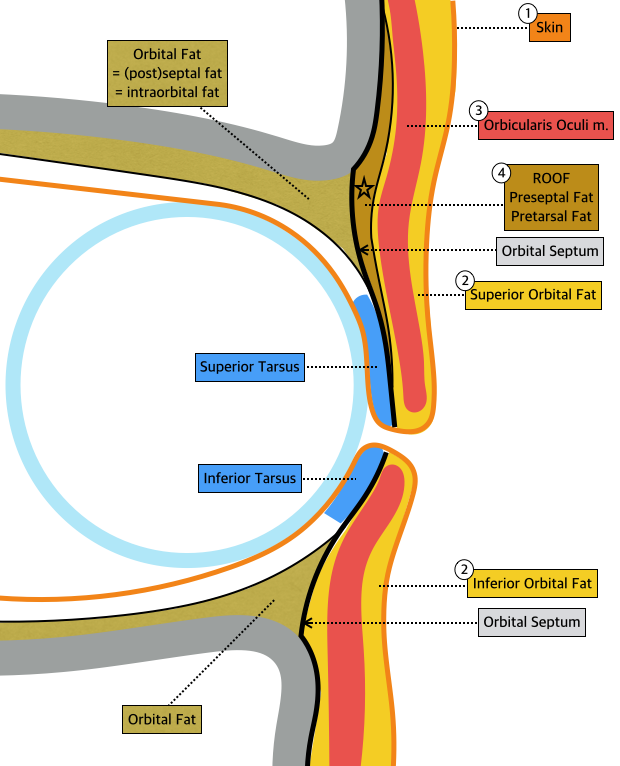
Image 1. Anatomy of upper and lower eyelids.
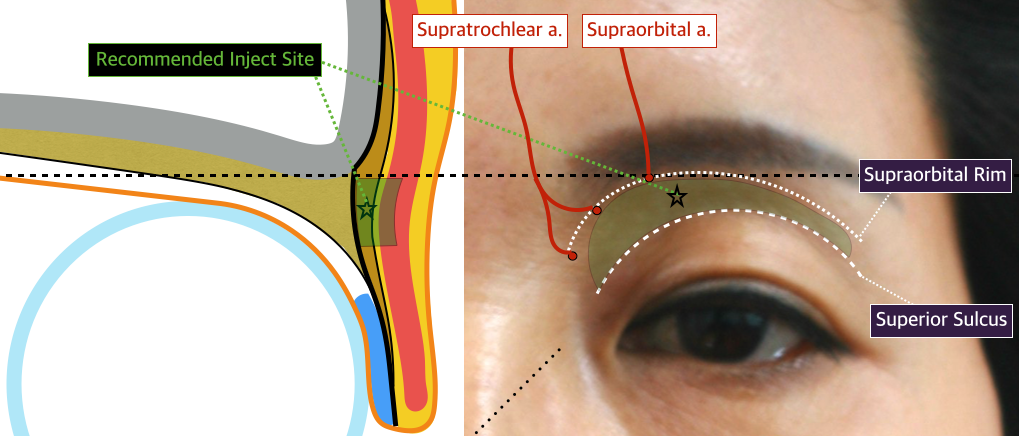
Image 2. Recommended injection site for sunken eyelid.
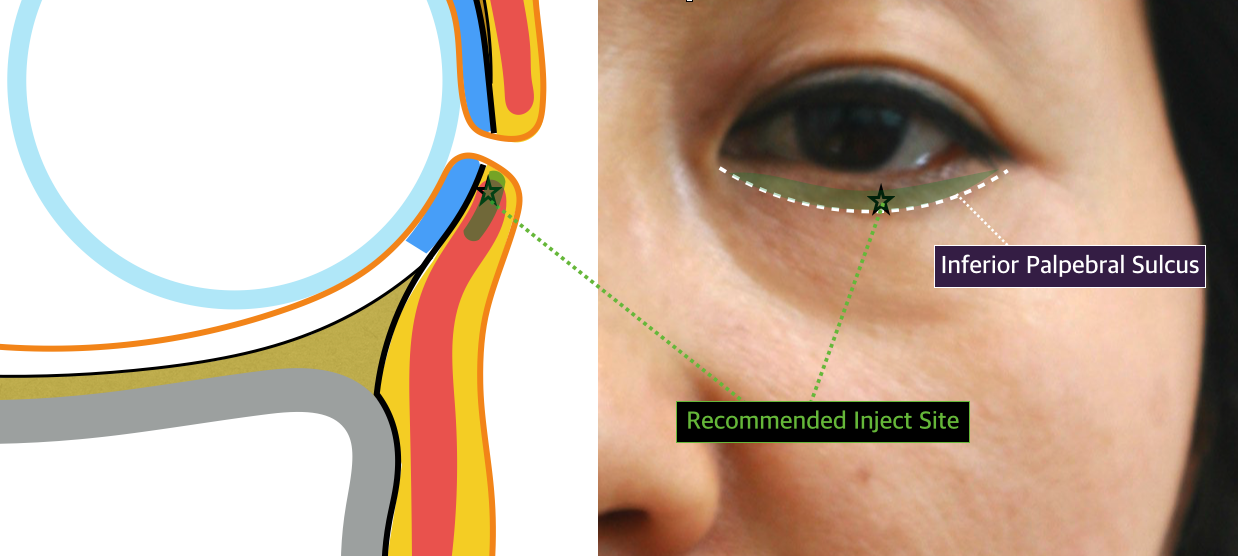
Image 3. Recommended injection site for pretarsal fullness.
[Advertisement] A-One LITE(Facial Diagnosys System) – Manufacturer: BOMTECH(www.bomtech.net)
References
1. Lin TM, et al. Application of Microautologous Fat Transplantation in the Correction of Sunken Upper Eyelid. Plast. Reconstr. Surg. Glob Open 2:e259, 2014.
2. Liew S. Nonsurgical Volumetric Upper Periorbital Rejuvenation: A Plastic Surgeon’s Perspective. Aesth. Plast. Surg. 35:319, 2011.
3. Park SK, et al. Correction of Superior Sulcus Deformity With Orbital Fat Anatomic Repositioning and Fat Graft Applied to Retro-Orbicularis Oculi Fat for Asian Eyelids. Aesth. Plast. Surg. 35:162, 2011.
4. Chen MC, et al. Anthropometry of Pretarsal Fullness and Eyelids in Oriental Women. Aesth. Plast. Surg. 37:617, 2013.
5. Kim YK, et al. Evaluation of Subciliary Incision Used in Blowout Fracture Treatment: Pretarsal Flattening after Lower Eyelid Surgery. Plast. Reconstr. Surg. 125:1479, 2010.




















