7. Skin necrosis
1) Skin necrosis is caused by the presence of ischemia and hypoxia in the healing wound. In other words, it is an iatrogenic error that induces circulatory disturbance from the bottom of the wound. Other known causes are as following.
① Excessive tension on the wound: insufficient dissection, incorrect surgery design, progressively enlarging hematoma or seroma
② Infected tissues
③ Tissues devitalized by excessive electrocautery
④ Overly extensive epidermal dissection
⑤ Wrong flap design: Flap with insufficient or unstable blood flow
⑥ Smoking
[Advertisement] MAGNUM(Q-switched Nd:YAG Laser) – Manufacturer: (www.i-dana.com)]
2) Relationship between flap necrosis and smoking
If a patient receiving, for example, melolabial interpolation flap abstained from smoking immediately after surgery but resumed in 1-2 weeks, flap necrosis can occur (Image 4). Smoking induces vasoconstriction through the action of nicotine and constriction of capillaries by stimulating the sympathetic nerve. Smoking hinders provision of oxygen to tissues and collagen deposition. One inhalation of a lit cigarette is known to cause approximately 9 minutes of vasoconstriction. When a patient smoking one pack a day receives flap technique or full-thickness skin graft, the risk of necrosis rises three times. Therefore, abstinence from smoking is necessary from 2 days before surgery to 1 week after.
3) Measures to tackle skin necrosis
A. There are no known solutions for preventing progression of skin necrosis. Typical treatment involves necrosis debridement, prevention of infection and secondary closing.
B. Prevention
1. Correct and appropriate planning
2. Close attention to hemostasis
3. Dissection of appropriate degree and width
4. Closure methods for reducing post-surgery edema
- Use of high-elasticity suture materials (prolene, nylon)
- Running suture technique, etc.

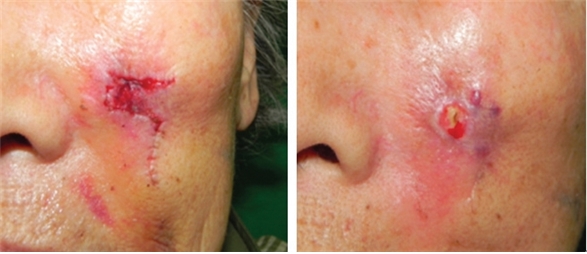
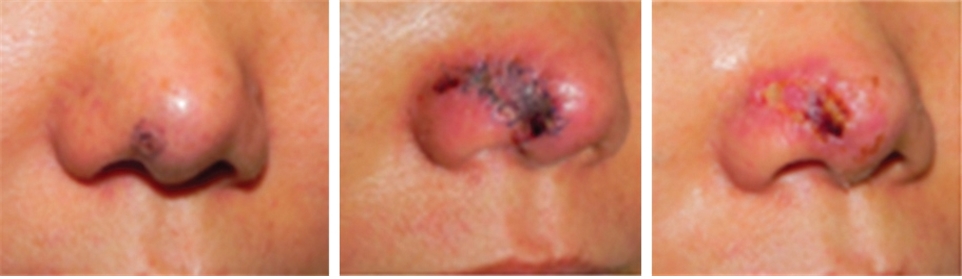
Image 4. Partial necrosis after flap technique (A. Interpolation flap B. Rhomboid flap. Island flap).
-To be continued-