8. Ectropion of the eyelid
To prevent ectropion, one should be well-versed in Snap test which evaluates the elasticity and laxity of the lower eyelid. Pull the lower eyelid with the thumb and index finger and lightly pull away from the globe. Young patients have good elasticity and when the lower eyelid is released, it returns to the original position immediately. This indicates a low risk of ectropion. Measures to tackle ectropion include medial canthopexy, lateral tarsorrhaphy, wedge excision, skin graft, and local flaps, etc. It is advisable to receive treatment from an ophthalmic plastic surgeon. Medial ectropion is particularly associated with a high risk of lacrimal dysfunction and cosultation with ophthalmology is necessary.
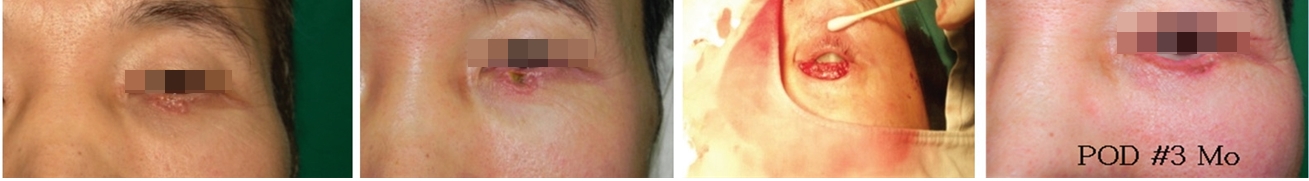
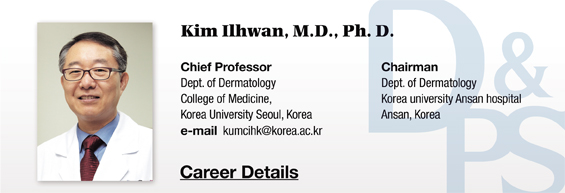
Image 5. Pigmented basal cell carcinoma of the lower eyelid was removed with Mohs surgery followed by dissection and simple suture. Ectropion did not occur. This patient was Snap test positive.
9. Scar and keloid
Hypertrophic scar and keloid are pathological reactions to tissue damage such as surgery. Hypertrophic scar refers to a raised scar due to excessive buildup of collagen within the original scar. Keloid is characterized by extensive scarring beyond the boundaries of the original scar. Both conditions can cause aesthetic and functional problems. They are more common in the chest area, black skin, and secondary closing (Image 7), etc. Hypertrophic scars occur 4 weeks after surgery and stabilize naturally never to recur. Keloids appear months after surgery, are not naturally resolved and continue to recur. Current treatments including steroid injection into the lesion, silicone gel sheeting and non-silicone wrap therapy, etc. show partial response in some lesions. Vascular laser (585, 595nm pulsed dye) therapy can improve the shape and symptoms but outcomes vary. Other treatments that can be tried in keloid include topical retinoid, imiquimod, cryosurgery, compression therapy, recombinant interferon gamma and interferon alpha-2b, and radiotherapy (low-dose ionizing radiation), etc. Injecting steroid in the lesion during and after surgery as part of resurgery of the scar can be effective.
[Advertisement] Tulip(Skin Tightening & Lifting) – Manufacturer: DANIL SMC(www.danilsmc.com)
In conclusion, the current and previous articles provided a review of major complications in dermatologic surgery, their causes and solutions. We can see that a lot of these complications can be prevented with knowledge of causal factors, presentations and prevention measures. Therefore, it is necessary to continue long-term follow up of patients to extend one’s clinical experience. I believe that the essence of medicine lies in continuous effort to solve problems. The answer lies in one’s effort to develope skills through extensive experience.
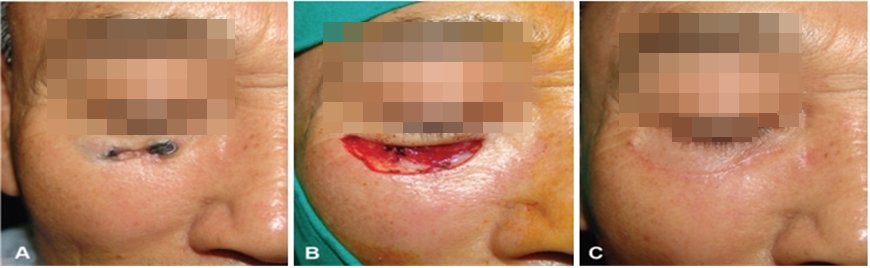
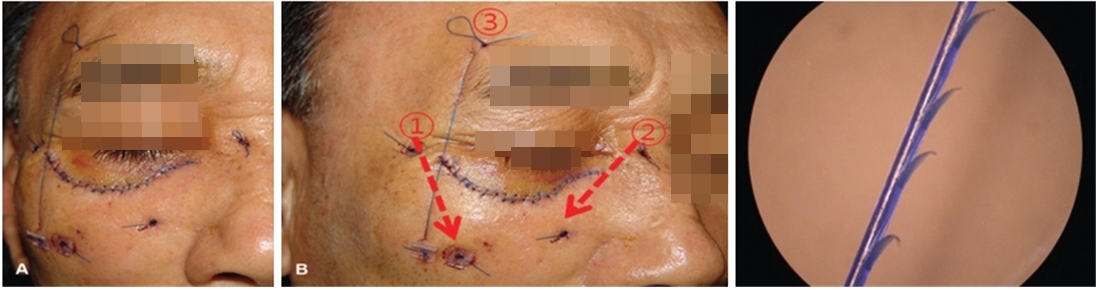
Image 6. The reconstruction technique I used for reconstruction of the skin defect resulting from Mohs surgery of pigmented basal cell carcinoma; to prevent ectropion, 4-0 prolene suture thread was used for Barbed Suture Suspension Technique (See Reference).

Image 7. Hypertrophic scar developing after removal of congenital nevus of the back.
Reference
1. Keyvan Nouri, Complications in Dermatologic Surgery. 2010.
2. Brooke R. Seckel, Facial danger zones. 1994.
3. Kim IH, et al. Ophthal Plast Reconstr Surg, Vol. 27, No. 3, 2011.
4. Smith JB, Fenske NA. Cutaneous manifestations and consequences of smoking. J Am Acad Dermatol.
1996 May;34(5 Pt 1):717-32; quiz 733-4. Cutaneous manifestations and consequences of smoking.
5. Futoryan and Grande, Dermatol Surg, 1995 Jun;21(6):509-14. Postoperative wound infection rates in
dermatologic surgery.
6. Bencini, et al, Arch Dermatol, 1991 Sep;127(9):1357-60. Antibiotic prophylaxis of wound infections in
skin surgery.
7. Griego and Zitelli, Arch Dermatol, 1998 Jun;134(6):688-92. Intra-incisional prophylactic antibiotics for
dermatologic surgery.
-To be continued-