Figure 2. Various methods of scar removal
The core concept of laser scar removal lies in the laser-tissue interactions, which are largely categorized as photothermal, photochemical, and photomechanical. Among these, photothermal effect, which refers to direct delivery of thermal energy to target chromophores in the skin while minimizing damage to the surrounding areas, is the most important for the success of laser therapy.
To enable such effect, it is important to understand the thermal relaxation time (TRT). Laser energy absorbed into the skin raises the temperature of tissues as the light energy is converted to heat energy. The TRT refers to the period of time it takes for the peak temperature immediately after laser irradiation to drop by half. That is, the temperature of target chromophores gets raised during laser irradiation but falls to a half of the peak temperature as the heat dissipates to surrounding tissues in TRT.
Excessive heat from laser conducted to tissues surrounding target chromophores can cause damage. To limit the thermal effect to only target chromophores and avoid damaging healthy tissues, laser should be irradiated for a period of time shorter than the TRT.5
.jpg)
Table 1. TRT of chromophores.
Dermatologic laser experienced a breakthrough when Anderson and Parrish proposed the theory of selective photothermolysis in 1983.6 This led to development of lasers with pulse durations suitable for certain target chromophores. The continuous wave argon, CO2, Nd:YAG (1064) laser was the first laser used in scar removal.5,7 Nd:YAG (1064) laser prevented collagenesis and effectively induced charring of the lesion and infection of the sloughing tissues through direct photo-biological actions. However, effects reported in early studies were only short-lived and scars often recurred.5 The response rate of Nd:YAG(1064) laser was only 36~47%.4
Until the early 1990s, the 585nmm pulsed dye laser (PDL) was often used in port-wine stains or telangiectasia. In 1994, Alster reported 57-83% clinical improvement of erythematous hypertrophic scars following 1-2 PDL treatments.8
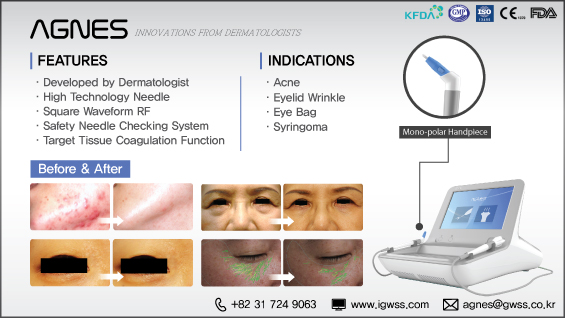
[Advertisement] AGNES(Radio Frequency) – Manufacturer: (www.igwss.com)
-To be continued
References
2. Wolfram D, Tzankov A, Pulzi P, Piza-Katzer H. Hypertrophic scars and keloids – A review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009; 35:171 – 81.
3. Groover IJ, Alster TS. Laser revision of scars and striae. Dermatol Ther. 2000;13:50 – 9.
4. Mustoe TA, Cooter RD, Gold MH, Hobbs FD, Ramelet AA, Shakespeare PG, et al., International Advisory Panel on Scar Management. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110(2):560 – 71
5. Nouri K, Alster TS, Ballard CJ, Vejjabhinanta V. Laser revision of scars. eMedicine Dermatology. 2008 [accessed 2009 December 22]. Available from: http://emdecine.medscape. com/article/1120673-overview
6. Anderson RR, Parrish JA. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524 – 7.
7. Niwa ABM, Mello APF, Torezan LA, Osorio N. Fractional photothermolysis for the treatment of hypertrophic scars: Clinical experience of eight cases. Dermatol Surg. 2009;35: 773 – 8.
8. Alster TS. Improvement of erythematous and hypertrophic scars by 585-nm fl ashlamp-pumped pulsed dye laser. Ann Plast Surg. 1994;32(2):186 – 90.