▶ Previous Artlcle : #14-2. Surgical Wound Coverage
Introduction (Classification, Figure 1)
Dermal substitutes are largely derived from two types of materials: fresh cadaver skin and artificial dermis developed from extracting collagen from bovine or porcine skin. The surgical grafting method can be divided into a two-stage or single-stage procedure. In the former, the split-thickness skin graft (STSG) is performed as a secondary procedure after waiting for successful engraftment of the artificial dermis. In the latter, the artificial dermis and STSG are applied simultaneously. The surgical method can be selected based on patient conditions and the wound environment to save on the high cost of dermal substitutes.
[Advertisement] MAGNUM(Q-switched Nd:YAG Laser) – Manufacturer: (www.i-dana.com)]
Currently available and clinically applied bioengineered dermal substitutes include Alloderm derived from cadaveric skin and Surederm developed in Korea. Completely synthesized products include Integra, first developed in the US from synthesized bovine collagen, Terudermis and Pelnac from Japan, and Matriderm recently developed in Germany.
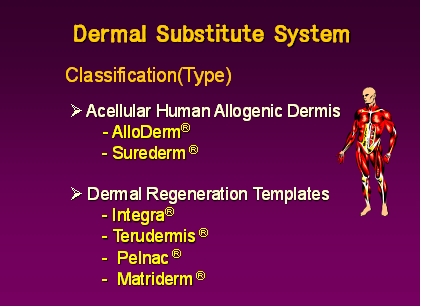
Figure 1-1. Classification (types of dermal substitutes).
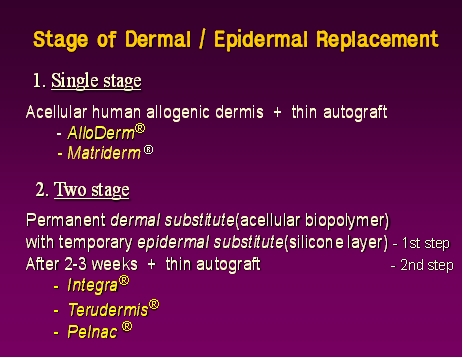
Figure 1-2. Classification (surgical methods).
Advantages of Artificial Dermis (Advantages, Figure 2)
a. Artificial dermis reduces scarring of the healing wound by reducing the inevitable contracture of the grafted STSG site and decreasing tension at the joints or other areas of the body with high mobility. This prevents functional impairment and minimizes contracture deformities.
b. Artificial dermis can provide immediate closure of the extensive wound (in the case of early excision and graft). This can improve the survival rate of patients with severe burn injuries.
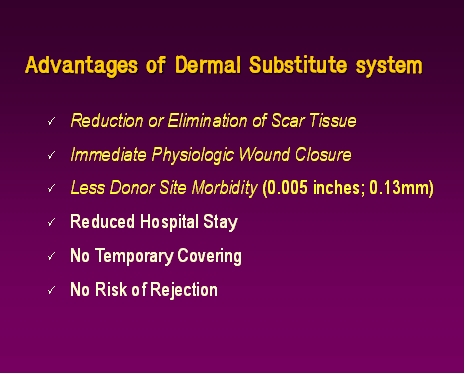
Figure 2. Advantages of the artificial dermis.
c. Using ultra-thin split thickness skin can decrease donor site morbidity (Figure 3).
d. In burn care, early removal of eschar and wound coverage provides early mobilization, thereby shortening hospitalization. This also allows early implementation of rehabilitation and can offset the biggest drawback of artificial dermis, its high cost.
e. Unlike other dressing materials, artificial dermis provides permanent wound coverage and does not require secondary surgery. Thus, unlike dressing materials that are removed after their purpose has been served, the artificial dermis acts as both wound protection and as a type of skin graft. Therefore, it is necessary to clearly establish scientific and legal evidence as well as indications for each classification when developing new materials or determining insurance coverage.
f. Artificial dermis has proven to be safe, and there have been no clinical cases of rejection.
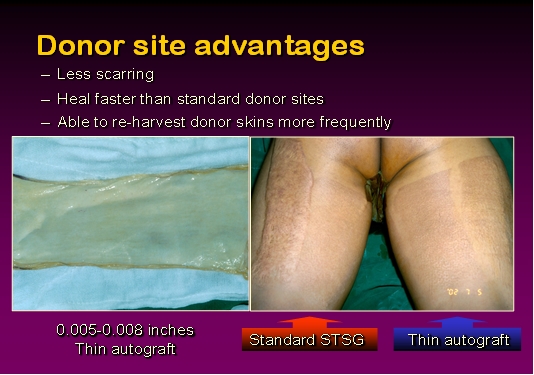
Figure 3. As STSG is harvested in the thickness of 5~8/1000 inches, which reduces donor site morbidity.
-To be continued





















