▶ Previous Artlcle : #2-1. Port-wine Stain
Histopathological Characteristics
The number of vessels appear to be increased due to vessel dilation and tortuosity rather than the actual increase in number, although the number of vessels may increase in some cases. In the same patient, other lesions may present increased number of normal capillaries. Through special staining, abnormalities in the distribution of nerves innervating the vessels can be seen. As it is not an actual tumor, it is not characterized by proliferation of vascular endothelial cells.
Associated Conditions
[Advertisement] FCR® (Fractional Prickle CoralCalcium Regentron) – Manufacturer: (www.thermoceutical.asia)]
In rare cases, port-wine stains can be accompanied by systematic conditions including eye, brain & nervous system anomaly, limb asymmetry or hypertrophy. There are a few syndromes whose association with port-wine stains have been established.
1) Klippel-Trenaunay syndrome
This congenital condition is characterized by capillary-lymphaticovenous malformation and hypertrophy of the affected limb. Limb hypertrophy can be congenital or occur around puberty. It can affect various areas of the body, but the lower limb is affected in 95% of cases. When local hypertrophy worsens with age, skin ulcer due to impeded circulation, soft tissue infection due to lymphedema, as well as bleeding and phlebothrombosis can occur. Venectasia in the form of varicose veins and limphedema are often observed in the affected limb.
2) Sturge-Weber syndrome
A type of neuro-oculocutaneous syndrome, Sturge-Weber syndrome is characterized by port-wine stains in the V1 branch of the trigeminal nerve (ophthalmic branch), ipsilateral leptomeningeal capillary-venous malformation, calcification in the choroid plexus and parenchymal venous perfusion defect. Cerebral invasion can cause epilepsy, neural damage and mental retardation.
3) Phakomatosis Pigmentovascularis (PPV)
PPV is a syndrome where malenocyte abnormality coexists with vasomotor nerves originating from prenatal neural crest. Capillary malformations appear in the trunk and lower limbs along with brown macules, pigmentary lesions, nevus spilus, abnormal mongolian spots. It can be accompanied by muscular, neurological, and ocular abnormalities.
Diagnostic Examinations
History taking: Check for existence at birth, growth in size, bleeding or ulceration, etc. to exclude the possibility of hemangioma or AVM. Vascular malformations are often present at birth and do not grow drastically in size later in life. In most port-wine stains, bleeding or ulceration are not observed.
Visual inspection: Visually examine the anatomical distribution, coloration, and other accompanied anomalies. Salmon patches are often located in the center of the forehead or occiput.
Palpation: Examine if the lesion is warmer than the surrounding normal skin or if the pulsation can be felt. AVM is clearly warmer and pulsation can be felt in some cases.
Biopsy: Biopsy is not required in typical lesions, however, it can be performed to examine the vessel thickness and depth as well as screen for hemangioma or AVM.
Radiological examination: This is not compulsory, but in the case of nontypical presentations such as presence of warmth, pain, bleeding, etc., AVM, Parkes Weber syndrome, and fast flow malformations such as progressive hemangioma, Doppler ultrasound can be used to screen for theses lesions. MRI can be considered in lesions invading the upper and inner eyelid to screen for cerebral invasion of Sturge-Weber syndrome.
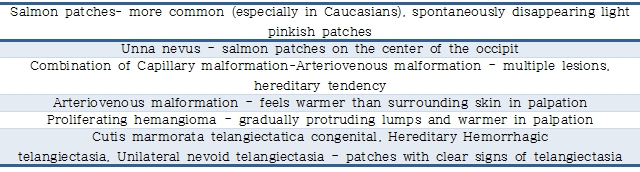
Diagnostic screening (See Table 1) Table 1. Differential diagnosis of port-wine stains and characteristics of each condition
Complications
A major concern for most patients is the disfigured appearance. In particular, lesions appearing in the face cause serious psychological distress. Hypertrophy in soft tissues and bones may cause gait disturbance or limphedema. As time progresses, protruding nodular lesions such as granuloma pyogenicum may appear and create further aesthetic problems.
Treatment
In the past when laser technology was not as advanced as today, electrocoagulation, cryotherapy, or make-up (camouflage) were used. Currently, Pulsed Dye Laser(585, 595nm), Long Pulse Nd:YAG Laser, KTP Laser, or Diode Laser, etc. which can destroy capillaries are being used. Since capillary malformations of the face can cause serious aesthetic problems, early initiation of treatment in younger ages can bring better outcomes as well as provide sociopsychological relief.
Due to advances in medicine and laser technology, port-wine stains, once considered a treatment-resistant vascular malformation, can be treated to some extent. Patients are therefore advised to seek for professional medical opinion for accurate diagnosis and initiation of optimal treatment.
References
❶ Boon LM, VikkulaM. Vascular malformations. In: Fitzpatrick’s Dermatology in General Medicine, 8th ed. New York: McGraw Hill, 2012:2076-2094. ❷ Chen JK, Ghasri P, Aguilar G, van Drooge AM, et al. An overview of clinical and experimental treatment modalities for port wine stains. J Am Acad Dermatol. 2012 Aug; 67(2):289-304.
-To be continued-
▶ Next Artlcle : #3-1. Treatment of Port-wine Stains