DISCUSSION
There is a clear demand for Laser treatment of various vascular lesions, but there are still challenges when using Laser energy in a therapeutic context. PDL and IPL are used to treat superficial vascular lesions, but are not ideal for treating deeper lesions.3 With the advent of Lasers with longer pulse durations and wavelengths than those used for PDL and IPL, deeper and larger caliber vessels can be managed more effectively without frequent treatment sessions and side effects. Long-pulsed Nd:YAG Laser treatment of deeper vessels has been shown to be effective; however, the long-term effects of this Laser treatment have not been evaluated.4 In this study, we demonstrated that diverse vascular lesions responded favorably to long-pulsed Nd:YAG Laser therapy. As expected, we found that selective photothermolysis of vessels in vascular disorders including erythema, telangiectasia, port wine stain, cherry angioma, and hemangioma could be achieved by 1064 nm Nd:YAG Laser pulses. Both PGA scores and patient satisfaction ratings after Laser treatment were good. Long-pulsed Nd:YAG Laser therapy can therefore potentially be used to treat both superficial and deep vascular disorders.
Among the Lasers for vascular lesions, the ratio of melanin to blood absorption is similar at 585 and 1064nm, whereas the absolute values of absorption and scattering coefficients are considerably lower at 1064nm as compared with 585nm.7,8 It might imply that 1064nm pulses can treat deeper vessels selectively. Lower absolute values of blood absorption at 1064nm can be compensated for by increasing the fluence. Although a very high fluence of more than 150J/cm2 must be applied, this increase in treatment fluence does not necessarily damage the epidermis, because the absolute absorption of melanin is lower at 1064nm as well.4 In addition, the absorption coefficient of blood at 1064nm is 0.4/mm, which is much higher than that of the surrounding dermis(0.05/mm) at the same wavelength. This difference in absorption coefficients makes 1064 nm light more selective for treatment of deep blood vessels than shorter wavelengths of light.8,9
There are several possible causes for the steep fluence-response curve of Nd:YAG Laser treatment. When blood is heated to 50-54oC, partial oxidation of oxyhemoglobin leads to met-hemoglobin(met-Hb) formation.7,10 Optical absorption by met-Hb is much higher than that of either Hb or hemoglobin.11,12 Several in vitro studies13,14 have demonstrated that when blood is photocoagulated by 1064 nm Nd:YAG Laser pulses, absorption at 1064 nm increases on the millisecond time scale by a factor of about 3, which may be due to partial conversion of oxyhemoglobin to met-Hb. When the lumen is thermally coagulated, optical scattering is increased and formation of a coagulum results in concentration of chromophores.1 In summary, long-pulsed Nd:YAG Laser irradiation can heat up the entire vessel wall and coagulate the vessel at high fluence, which aids in the clearance of vascular lesions, unlike PDL and IPL.
With regard to side-effects, higher risk of potential collateral damage around vessels and pain during the procedure should be kept in mind when using this Laser for vessels.2 Water, a competing chromophore of light at the wavelength of 1064 nm, may be the culprit responsible for additional tissue damage despite the fact that this wavelength is absorbed 10-fold more by oxyhemoglobin than water.2 In our study, all patients tolerated the procedure moderately well without remarkable pain. Two patients experienced post-inflammatory hyperpigmentation on the site of the vesicles; this epidermal damage may have been caused by the high fluence. Technically, a non-overlapping technique is very important to avoid subsequent complications like scar formation.15 When we performed Laser therapy to treat telangiectatic vessels, we evaluated the therapeutic end point based on the immediate response of the vessels. However, when treating diffuse erythema rather than telangiectasia, clinicians should be cautious when selecting parameters; however, guidelines to reduce adverse reactions have yet to be established.
This study had several limitations. First, we included only a small number of patients. Second, this was not a randomized controlled study and we did not directly compare the long-pulsed Nd:YAG Laser with PDL and IPL. Third, long-term follow-up was not performed.
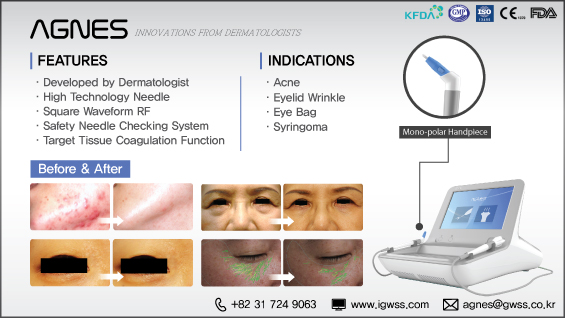
[Advertisement] AGNES(Radio Frequency) – Manufacturer: (www.igwss.com)
Nevertheless, we demonstrated that long-pulsed Nd:YAG Laser treatment is an alternative treatment modality for various vascular problems recalcitrant to standard therapy. Our study could also contribute to the establishment of appropriate treatment parameters. It is important to note that the use of bulk skin cooling, no overlapping of pulses, use of subpurpuric fluences, and use of a small spot size can limit dermal injury and improve the safety of Nd:YAG Lasers. Further studies comparing the effects of variations in each of the treatment parameters or different treatment intervals should be performed to determine optimal treatment conditions.
REFERENCES
4. Yang MU, Yaroslavsky AN, Farinelli WA, Flotte TJ, Rius-Diaz F, Tsao SS, et al. Long-pulsed neodymium: yttrium-aluminum-garnet Laser treatment for port-wine stains. J Am Acad Dermatol 2005;52:480-90.
5. Civas E, Koc E, Aksoy B, Aksoy HM. Clinical experience in the treatment of different vascular lesions using a neodymium-doped yttrium aluminum garnet Laser. Dermatol Surg 2009;35: 1933-41.
6. Ozdemir M, Baysal I, Engin B, Ozdemir S. Treatment of angiokeratoma of Fordyce with long-pulse neodymium-doped yttrium aluminium garnet Laser. Dermatol Surg 2009;35:92-7.
7. Seto Y, Kataoka M, Tsuge K. Stability of blood carbon monoxide and hemoglobins during heating. Forensic Sci Int 2001;121:144- 50.
8. Anderson RR. Optics of the skin. In: Lim HW, Soter NA, editors. Clinical photomedicine. New York: Marcel Dekker; 1993. p.13-35.
9. Landthaler M, Haina D, Brunner R, Waidelich W, Braun-Falco O. Neodymium-YAG Laser therapy for vascular lesions. J Am Acad Dermatol 1986;14:107-17.
10. Randerberg L, Daae HA, Svaasand L. Optical properties of human blood as a function of temperature. In: Bartels KE, editor. Lasers in surgery: advanced characterization, therapeutics, and systems XII. Bellingham: Society of Photo-optical Instrumentation Engineers; 2002. p.20-8.
11. Kuenstner JT, Norrish KH. Spectrophotometry of human hemoglobin in the near infrared region from 1000 to 2500 nm. J Near Infrared Spectroscopy 1994;2:59-65.
12. Zjilstra WG, Buursma A, Van Assendelft OW. Journal of Near Infrared Visible and near infrared absorption spectra of human and animal haemoglobin: determination and application. Utrecht: VSP Publishing; 2000.
13. Barton JK, Frangineas G, Pummer H, Black JF. Cooperative phenomena in two-pulse, two-color Laser photocoagulation of cutaneous blood vessels. Photochem Photobiol 2001;73:642- 50.
14. Barton JK, Wade NH, Black JF. Dynamic optical properties of blood irradiated at 1064 nm. Laser Surg Med 2003;32 Suppl 15:31.
15. Kono T, Frederick Groff W, Chan HH, Sakurai H, Yamaki T. Long-pulsed neodymium: yttrium-aluminum-garnet Laser treatment for hypertrophic port-wine stains on the lips. J Cosmet Laser Ther 2009;11:11-3.
-To be continued