Thhis is Dr. Kim`s opinion. Please read it and tell your opinion.
1. What could be the correct diagnosis?
The present case could be diagnosed as any of the following; café-au-lait spot, Becker's nevus, Ota’s nevus, or laser induced post-inflammatory hyperpigmentation (PIH), etc.
The image of the first visit shows a brown spot with somewhat mottled coloring and relatively clear boundaries. Its distribution is along the facial nerve but the clear lack of blue coloring rules out Ota’s nevus. Moreover, the patient has no family history of neurofibromatosis to confirm café-au-lait spot. I saw that the lesion was most likely Becker’s nevus due to its extensive size and inconsistent coloring. Café-au-lait spot and Becker’s nevus show clinical differences as shown in <Table 1>.
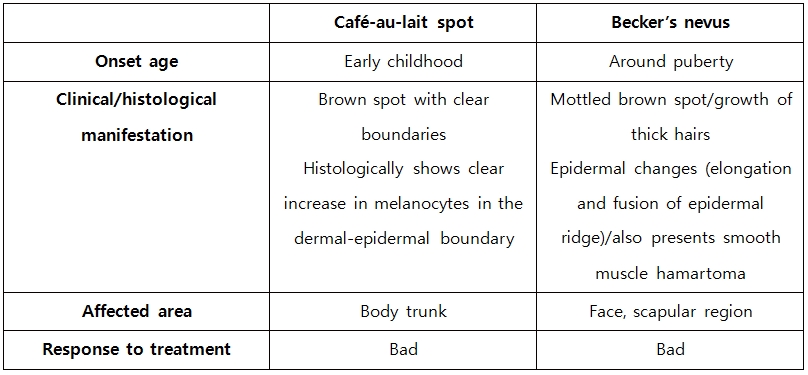
Table 1. Differences between café-au-lait spot and Becker’s nevus.
[Advertisement] MAGNUM(Q-switched Nd:YAG Laser) – Manufacturer: (www.i-dana.com)]
Outside what is discussed in the textbooks, domestic literature on the condition include ‘Clinical and Histopathological Study on Becker’s nevus’ published by Lee et al. in 1993, as well as ‘Clinical and Histopathological Examination of Becker’s melanosis‘ published by Oh et al. in 1994. Both reports included a number of early childhood cases similar to the present case. However, the two studies were retrospective reviews of medical charts and relied on the patients’ testimonies. It is, therefore, difficult to clarify if the disease developed during early childhood. It would have helped diagnosis if biopsy had been conducted.
Biopsy is rarely carried out in pediatric patients aged 4 years. However, the boundaries and color of the lesion do not seem to agree with those of Becker’s nevus. The question I would like to ask is, even if biopsy is carried out in such a young patient, would it clearly show the fusion of epidermal ridges that characterize Becker’s nevus? Most of the studies are limited to adult patients.
I summarize as following.
* It should be understood that clear diagnosis of epidermal hyperpigmentation of the face is often difficult. Many case studies coin new terms to report cases that evade clear diagnosis.
* Laser and treatment related hyperpigmentation can be considered. However, with the current patient, I allotted a long period of time between treatments for observation but no spontaneous improvement was seen. As the patient approaches puberty, pigments seem to darken. Therefore, it is unlikely that this case is continued hyperpigmentation from excessive laser use.
* The current conditions of the lesion resemble the coloring and location of erythromelanosis. But at the same time, there are no signs of keratosis pilaris.
* In conclusion, biopsy should be recommended to help more accurate diagnosis and determine an appropriate treatment course based on the results.
2. Is early treatment more effective?
Different treatment guidelines are available for various congenital vascular and pigment lesions, etc. Many experts tend to agree that treatment initiated in the early ages is more effective. Especially, laser treatment is more efficient and financially less burdensome when applied early. In this light, early treatment was thought to benefit the present case more. However, Becker’s nevus develops around puberty and is characterized by growth of thick hairs on the site of the lesion. Based on these characteristics, the condition is theorized to fully manifest from the influence of sex hormones.
With this patient, the treatment began in early childhood and temporary improvement was seen. Recently, however, the lesion is darkening. I suspect that this darkening of the lesion can be attributed to puberty as the patient is 10 years old now. Therefore, I view that Becker’s nevus could be categorized as a disease that does not benefit from early treatment.
3. Was it wise to select 532nm Q-switched laser as the first line therapy?
Reports of extensive laser treatment of Becker’s nevus are only few and far between. The 532nm Q-switched Nd:YAG laser or 694nm Q-switched ruby laser is reported to be mainly used. Other treatments such as 755nm long pulse alexandrite laser, Er:YAG resurfacing, or cryotherapy, etc. have been reported to be effective, however, the evidence is anecdotal. According to a Korean publication in 2004 ‘Clinical evaluation of efficacy of Nd:YAG laser on Becker’s nevus’ by Kim et al., the 532nm Q-switched Nd:YAG laser’s efficacy is 50%. Moreover, out of 3 cases of Becker’s nevus of the face, only 1 responded well, indicating that facial lesions are as refractory as trunk lesions.
In 2009, Choi et al. tried 755nm long pulsed alexandrite laser therapy in 11 patients with Becker’s nevus and observed good response in about 70% of patients.
Long pulse therapy, resurfacing and other alternatives were tried in the present case to no avail. This may be due to the limits of early treatment. Alternately, it would have been better to try long pulse or Er:YAG first and use Q-switched Nd:YAG to tackle remaining lesions with better precision.
Additionally, more analytical data on cases with facial Becker’s nevus are needed.
I would greatly appreciate if other specialists shared their opinions on this topic.
-The end-