▶ Previous Artlcle : #2-2. The Etiology of Vitiligo: Autoimmune Theory and Neurohumoral Theory
In general, vitiligo lesions of the skin appear as depigmented macules which are clearly distinguished from surrounding skin.
Vitiligo is classified in various ways depending on its clinical presentations. Textbook of Dermatology 5th Edition, used as a key reference in medical schools of Korea, categorizes vitiligo into Korean type, universal type and general type (Table 1). However, the newly released Fitzpatrick’s dermatology in the general medicine 8th Edition classifies vitiligo into two large categories depending on distribution, range and number of macules on the skin.
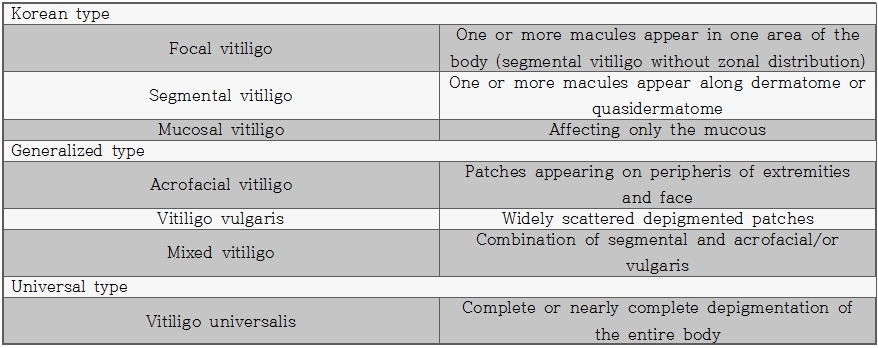
Table 1. Classification of vitiligo according to Textbook of Dermatology 5th Edition
One method of classification divides vitiligo largely into; generalized, universalis and localized. Generalized vitiligo is subdivided into vitiligo vulgaris, acrofacial vitiligo and mixed vitiligo. Localized vitiligo is subdivided into focal, segmental, and mucosal vitiligo. Another method of classification divides vitiligo into segmental and nonsegmental depending on clinical features and natural progression of disease. This method includes localized, generalized and acrofacial types into nonsegmental viltiligo. Fitzpatrick’s dermatology in the general medicine 8th Edition provides the following definition of each type.
[Advertisement] Ultra Skin/Pastelle – Manufacturer: WONTECH(www.wtlaser.com)
•Vitiligo vulgaris: the most common form of generalized vitiligo. Depigmented macules tend to appear symmetrically on each side of the body although the degree of symmetry may vary.
•Acrofacial vitiligo: This subtype of generalized vitiligo appear in periphery of fingers and periorificial areas of the face.
•Mixed vitiligo: appears in a combination of vitiligo vulagaris and acrofacial, or segmental and acrofacial types.
•Vitiligo universalis: Depigmentation encompasses most of the body and is the most severe form of vitiligo.
•Focal vitiligo: One or a few scattered macules appear in one area of the body, however, unlike segmental vitiligo, it does not have dermatomal distribution. It is sometimes considered as premonitory symptoms of generalized vitiligo.
•Mucosal vitiligo: depigmentation of only the mucous membranes
•Segmental vitiligo: Depigmented macules appear unilaterally along the dermatome, without crossing over the center line of the body. It mostly affects children and does not progress into generalized vitiligo. The Macules may last a few years without changing in size. Unlike generalized vitiligo, it is rarely associated with autoimmune disorders.
Besides the common classes of vitiligo listed above, there are also unusual variations of the disease as follows.
•Trichrome vitiligo: characterized by existence of a ring-shaped, tan area between normal and totally depigmented skin (Figure 1). •Quadrichrome vitiligo: often affects dark skin. Trichrome lesions exist and a fourth color of dark brown appear at sites of perifollicular repigmentation.
•Pentachrome vitiligo: Fives colors of lesions appear; (from inside) white, yellow-brown, brown, dark brown and black.
•Confetti vitiligo or Vitiligo ponctué: characterized by small confetti-like macules that may scatter over normal or hyperpigmented patches of the skin.
•Red vitiligo: characterized by protruding depigmented lesions with erythemic boundaries.
•Blue vitiligo: Histologically, melanin is absent in the epidermis but a large number of melanophages in thedermis cause blue-grey lesions (Figure 2).
I often encounter patients with aggravated conditions due to excessive exfoliation during a shower or bath. Therefore, to successfully treat vitiligo it is important for both the doctor and patient to be well-acquainted with factors of prognosis and deterioration and minimize impact of environmental factors. Many factors that may exacerbate Vitiligo include; physical damage to skin, sun burn, psychological stress, inflammation response, pregnancy, oral contraceptives, and Vitamin deficiency, etc. However, specific environmental factors causing vitiligo have not been identified.
Prognosis is poor in patients with family history of vitiligo, mucosal lesions, Koebner phenomenon or nonsegmental vitiligo. On the contrary, patients with disease onset at a young age, recent development of lesions, dark skin, or lesions on the face, neck and body truck, etc. tend to have positive response to treatment, whereas lesions appearing in extremities are very difficult to treat.

Figure 1. Trichrome vitiligo
-To be continued-
▶ Next Artlcle : #3-2. Diseases associated with clinical presentations