▶ Previous Artlcle : #2-1. Thermal Effect and Non-Thermal, Non-Cavitational Effect of Ultrasound
Like an electromagnetic wave, ultrasound is reflected on the boundary between different media. Ultrasound will pass through the boundary, without reflection, if the two tissues have identical density and propagation velocity, but will be reflected on the boundary between two tissues with different density or propagation velocity and thus different impedance.
[Advertisement] Reandnè Thread Series – Manufacturer: GTG KOREA(www.gtgkorea.com)
For example, ultrasound reflection rarely occurs between muscle and fat, which have almost no difference in impedance, as is the case between skin and fat. Muscle and bone, on the other hand, have a great difference in impedance, reflecting 30% of ultrasound energy, which is also the case between periosteum and bone, where 70% of the energy is reflected. The longitudinal waves of ultrasound is shifted to transverse waves between periosteum and bone due to the drastic difference in density, generating a shearing force. The shearing force creates a heat energy, causing an intensive temperature rise in the periosteum, where the heat cannot be dispersed well due to the low vascular distribution. This may cause periosteal pain by heat injury to the periosteum.
The concentrated heat caused by impedance difference between two media is clinically very important. In particular, dermatological devices that require a external contact between skin and the transducer may create heat injury on the surface of the transducer due to reflection, inducing perforation or a burn on the skin, if there is air between the contact surfaces.
The reflectance is low when the angle between the incident direction of the ultrasound energy and the contact surface is 90 degrees, but heat concentration by reflection occurs, possibly causing a burn, when the angle becomes closer to 45 degrees. The reflectance on the boundary between each tissue is summarized in <Table 3>.
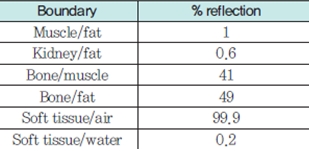
Table 3. % reflection on the boundary between each tissue
Such a thermal mechanism by ultrasound is relatively well-known, and many studies have investigated the temperature rise by exposure to various media. Based on these evidences, temperature rise can be estimated using a mathematical model.
If one knows the temporal-average intensity (ITA) of ultrasound at a certain point of tissue, then the mean heat production rate per unit time and per unit volume can be calculated as below:

In this equation, α is the ultrasound amplitude absorption coefficient, a constant depending on the frequency of ultrasound.
In the absence of heat loss, the maximum temperature rise, ΔTmax, is,
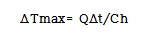
Δt is the irradiation time and Ch is medium-specific heat coefficient. As a biological tissue is close to water, Ch is 4.18 J/㎤℃. When the frequency of ultrasound is 5 MHz, α is approximately 0.25/cm·s, and if the ITA is 1 W/cm2, then Q is 0.5 J/㎤·s.
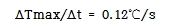
In other words, 5 MHz ultrasound irradiated for 1 second at the intensity of 1 W/㎠ can raise the tissue temperature by 0.12℃. If the maximum intensity of a diagnostic ultrasound device was 500 W/㎠, the maximum temperature difference per second would be 60℃/s. Because the pulse duration, Δt, of diagnostic ultrasound devices is mostly around 2 μs, the maximum temperature rise is 120 μ℃, supporting that diagnostic ultrasound devices cause very few heat injury. On the contrary, high-intensity focused ultrasound (HIFU) can increase the intensity as high as 5000 W/㎠, and thus temperature difference of 600℃/s. When the pulse duration is about 100m/s, the temperature rise will be about 60℃, at which point the tissue may be cauterized. A lot of experimental studies measuring the actual temperature rise in various mammalian organs and human biological tissues have also reported similar results to the above mathematical model. Further studies are ongoing to investigate whether it is clinically possible to raise the tissue temperature to a certain level and then maintain the temperature for a certain period of time.
In application of ultrasound in human body, the tissue temperature rise is important because, in terms of cytology, intracellular enzymes and metabolic activities are enhanced at around 40℃, but when the temperature rises beyond that (≥45℃) or after a long-term exposure, various proteins are denaturalized or coagulated and the enzymes and metabolic activities are reduced, ultimately damaging cellular function and structure. The results of various experiments on cells comprehensively suggest that cell death can be induced by exposure to the heat of 40℃ for 5-100 hours depending on the cell type, but no irreversible denaturization was reported below 40℃. Diagnostic ultrasound devices should be designed, therefore, not to raise the tissue temperature to beyond 40℃, and therapeutic ultrasound devices should be able to adjust the temperature rise and exposure time.
The extent of heat damage depends on the type of cell. In case of HeLa cells, for example, 100% cell death occurred after the exposure at 41℃ for 96 hours and after the exposure at 46℃ for 30 minutes. This idea can be referred to as 100% lethal dose (LD100). In case of sarcoma -180 tumor cell line, 50% cell death occurred after the exposure at 42℃ for 2 hours and after the exposure at 46℃ for 7.5 minutes, which can be referred to as LD50.
At the cellular level, this idea can be also applied to biological tissues. Because a number of studies are reporting the results from observation of tissue denaturization by exposure time at 43℃, the minimal exposure time at 43℃ before tissue starts denaturization is referred to t43, as a kind of cut-off value. The results of t43 studies in various tissues are summarized in <Table 4>.
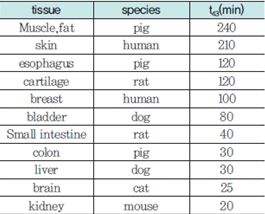
Table 4. Results of t43 studies in various tissues
These results suggest that each tissue has different absorption rate of ultrasound energy and thus different level of heat production by ultrasound energy. For example, tissues with a high content of collagen, such as bone and articular capsule, have a high absorption rate of ultrasound, and thus can be easily damaged by short-term exposure. Brain and nervous tissues are also vulnerable to damage due to their high absorption rate. On the contrary, skin and fat tissues have a low absorption rate and requires high frequency and sound wave intensity to increase the temperature. The absorption rate becomes almost multiplied to which the level is proportional to the frequency when the frequency is high and wavelength is short. That is, 3 MHz has an absorption coefficient approximately 3 times higher than 1 MHz in fat and muscle. Elevating frequency can be an option for raising the tissue temperature in skin, fat and muscle with a low absorption rate.
2. Non-Cavitational and Non-Thermal Effect
Several studies have investigated lung hemorrhage, one of the side effects of ultrasound, without a clear conclusion on the cause. Thermal effect could be eliminated from a possible cause, but there is still a controversy over whether cavitational effect could be the cause. The shearing force that moves or tears tissues by a radiating physical force is assumed to be a possible mechanism.
This mechanism of action explains the activation of tactile sense, auditory response and fetal movement, bone regeneration, tissue regeneration, retinodialysis and hemostasis. In addition, further studies are ongoing to find an explanation for the enhanced permeability for drug delivery by ultrasound, which cannot be fully explained by cavitational effect.
-To be continued-
▶ Next Artlcle : #3-1. Ultrasound Cavitation





















