▶ Previous Artlcle : #8. Pre-Surgical Knowledge Part II for Preparation of Skin Tumorectomy in the Out-Patient
Case
Patient: A 23-year-old woman
Chief complaint: Sweaty armpits (duration: > 6 years)
Past history and family history: Started during adolescence, and the father and his brother share the same symptom.
Skin and physical findings: She had pigmented axillary skin and dry bilateral cerumen and reported frequent use of topical antiperspirants for increased sweating and resultant odor while nervous, but no other symptoms were observed.
Examinations: Blood test was performed to differentiate secondary hyperhidrosis and Minor Test was used to confirm the activity of axillary sweat glands (Fig. 1).
Diagnosis: Primary axillary hyperhidrosis was diagnosed based on the above findings and examination findings.
Consultation: She visited the hospital for surgical removal to overcome the limitations of the local application of Driclor. She was informed of advantages and disadvantages of non-surgical therapies, but still wanted radical surgery.
Surgical procedure: Subcutaneous sweat glands were eliminated by subcutaneous tissue shaving procedure with minimal incision (see the right side).

Fig. 1. Minor Test
Discussion on the Treatment Modalities of Axillary Hyperhidrosis
Primary or essential hyperhidrosis is a condition with symptoms presented by excessive activation of the nervous system that controls perspiration (sudomotor: activated by acetylcholine at cholinergic nerve terminals of the sympathetic nervous system) without any apparent cause, while secondary hyperhidrosis refers to a condition associated with any specific cause including obesity, menopause, infection, antidepressant use, malignancy, neurologic disorder, endocrine disease (hypoglycemia, hyperthyroidism, etc.), spinal cord injury, chemical weapons (acetylcholinesterase inhibitors), and others. Sweat is clear, colorless liquid of pH 4-6.8, containing 98-99% water, NaCl, fatty acid, lactic acid and urea. Eccrine sweat glands are distributed in the skin throughout the body, but are predominant in hands, feet and axilla with normal morphology and function (Fig. 3).
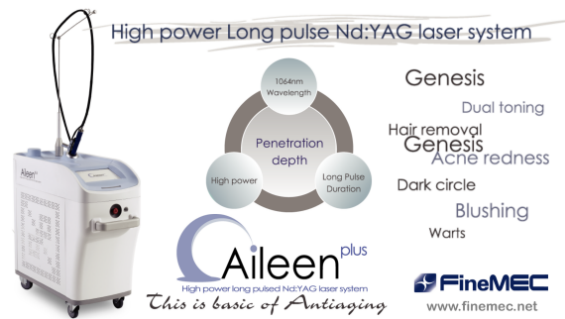
[Advertisement] ▶ Aileen plus(Long pulsed Nd:YAG Laser) – Manufacturer: FineMEC(www.finemec.net)
Normally, perspiration is controlled autonomously by the heat-regulating centers, independent of the level of consciousness, while is stimulated by emotion or stress in patients with hyperhidrosis. Hypersensitivity reaction to emotional stimulus from hypothalamus and cerebral cortex is currently deemed the primary abnormality in patients with hyperhidrosis, which is why it does not occur while sleeping or relaxed.
Axillary hyperhidrosis is clinically a type of primary (essential) focal hyperhidrosis. Other than palmoplantar hyperhidrosis, axillary hyperhidrosis is the most common type of hyperhidrosis, often presenting alone or accompanied by palmoplantar hyperhidrosis. According to data in the US, the prevalence of primary hyperhidrosis is 2.8%, of which half of them (1.4%) is axillary hyperhidrosis and 1/6 (0.5%) is the one causing limitations in daily activities. The diagnosis can be made quite easily by observing increased perspiration. The definite diagnosis is available by investigating the patient’s medical history, past history and family history and by conducting physical examinations. The perspiration area and activity can be confirmed by Minor Test (Fig. 1) using iodine-starch solution (Table 1).

Table 1. Iodine-Starch Solution (30 ml) Formula

Fig. 2. Botulinum Toxin Type A Injection: Intradermal injection at intervals of 1-2 cm, 50 U for each armpit.

Fig. 3. Morphological diagram (Left-eccrine, Right-apocrine) and histological features (Upper-eccrine, Lower-apocrine) of axillary sweat glands
-To be continued-
▶ Next Artlcle : #9-2. Surgical Treatment of Axillary Hyperhidrosis