▶ Previous Artlcle : #9-1. Surgical Treatment of Axillary Hyperhidrosis
Treatment: Stepwise Approach according to Symptoms
In the presence of symptoms by emotional and mental causes, systemic anticholinergics should be considered in consultation with a specialist. Otherwise, the patient should follow the stepwise treatment procedure as below:
[Advertisement] DEPILIGHT(808 Diode laser for Hair Removal) – Manufacturer: DANIL SMC(www.danilsmc.com)
Stage 1: In the absence of emotional and mental causes, topical antiperspirants (aluminum chloride hexahydrate, Drysol) ― 10-15% concentration for armpits and 30% for hands and feet ― are used. The skin condition should be checked due to its highly irritative nature. Upon the occurrence of irritation, the application should be discontinued and the irritation should be managed with topical steroids. If the irritation continues for more than 2 weeks, the patient should be referred to a dermatologist. Topical deodorants are only capable of reducing the bacteria causing the smell of sweat, not inhibiting perspiration. The timing of application is also important. Twice a day (morning and evening) or once a day (evening) application is more effective than morning application. In order to reduce skin irritation, the agent should be applied to a dry skin and washed with water 6-8 hours later. After shaving, should wait for 24-48 hours to use. Patients often cover the area with plastic wrap hopping to enhance the efficacy, but it rather increases irritation.
Stage 2: The following two methods can be considered for lesions not responding well to the stage 1 treatments.
A. Ionophoresis: This method is rarely used in clinical practice, because it is not easily applicable to axillary hyperhidrosis and the condition often recurs once the treatment is discontinued.
B. Botulinum Toxin Type A injection (Fig. 2): Botulinum Toxin Type A is approved for moderate continuous primary axillary hyperhidrosis that is resistant to topical therapies and interferes with daily activities. Clinical improvement appears within a week after injection. Sweat gland function is gradually recovered, and the therapeutic effect lasts for 7.5 months on average, although there is a difference between individuals. The cost is expensive, considering that the injection should be repeated every 4-17 months, but it does not entail side effects, such as compensatory hyperhidrosis.
Stage 3: Surgery
1) Current Surgical Procedures
A. The use of endoscopic thoracic sympathectomy is limited due to surgery-related complications, such as pneumothorax, and high risk of developing compensatory hyperhidrosis.
Extensive surgical excision of axillary tissues is seldom used now, because of long recovery time and high risk of complications, including infection/myocellulitis/fascitis, ecchymosis, hematoma, peripheral nerve injury (dysesthesia, sensoparalysis, etc.), peripheral vascular injury, secondary permanent malformation, aesthetic malformation or excessive atrophic scar, muscle injury or irritation, fat embolism, periostitis or osteomyelitis, and seroma.
2) Personal Preference: Surgery and Laser therapy
A. Surgery: Modified subcutaneous tissue shaving method with minimal incision (Fig. 4)
1) After local anesthesia with 0.5% lidocaine solution (1:200,000 dilution of epinephrine), a 1.5 cm incision is made parallel to the wrinkle line at 1/3 outside the axilla, followed by tissue dissection using Mesenbaum at the upper layer of fat, with hemorrhage control.
2) The fat layer in the hypodermis and subdermal tissue around the incision are removed using Mesenbaum (manual removal), and inside of the subdermal tissue is shaved with a modified Inaba’s device.
3) The tissue is removed until the philosebaceous unit appears (Fig. 5). After reconfirming hemorrhage, the skin and fat layer are bound together by quilting suture, and compressive dressing is applied for 3-5 days. Care should be taken because excessive removal may cause subdermal vascular plexus damage and resultant tissue necrosis.
B. Cauterization using a Long pulsed 1444 nm Nd:YAG Laser Fiber (Interstitial laser, Fig. 6)
This technique was developed based on the fact that sweat gland tissue consists of more than 20% of water and 1444 nm wavelength is well absorbed by water and fat tissue (x100 water absorption and x15 fat absorption compared to 1064 nm), and that a laser fiber can be used for a noninvasive procedure. This procedure can be performed on an outpatient basis under local anesthesia. A laser fiber is inserted through a 18 G needle hole, and point-by-point coagulation is performed for pores.

Fig. 4. A diagram of the subdermal target. All tissues from the upper layer of fat to immediately below the pilosebaceous unit should be removed for complete elimination of the sweat gland.

Fig. 5. Tissue should be removed until the pilosebaceous unit appears.
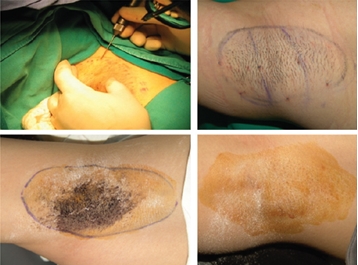
Fig. 6. Before, during and after the Interstitial laser procedure.
References
1. Eisenach JH, Atkinson JL, Fealey RD. Hyperhidrosis: evolving therapies for a well-established phenomenon. Mayo Clin Proc. 2005 May;80(5):657-66.
2. Stolman LP. Treatment of hyperhidrosis. Dermatol Clin. 1998 Oct;16(4):863-9.
3. Rusciani L, Severino E, Rusciani A. Type A botulinum toxin: a new treatment for axillary and palmar hyperhidrosis. J Drugs Dermatol. 2002 Sep;1(2):147-51.
4. Naver H, Swartling C, Aquilonius SM. Palmar and axillary hyperhidrosis treated with botulinum toxin: one-year clinical follow-up. Eur J Neurol. 2000 Jan;7(1):55-62.
5. Hwang KC, Kim IH. The Changes of the Barrier Function of Axillary Skin and the Quality of Life in the Patients of Axillary Hyperhidrosis after the Injection of
Botulinum Toxin A. Korean J Dermatol. 2004 Apr;42(4):406-412.
6. Kim IH, Seo SL, Oh CH. Minimally invasive surgery for axillary osmidrosis:
combined operation with CO2 laser and subcutaneous tissue remover. Dermatol Surg. 1999 Nov;25(11):875-9.
7. Lee GG, Lee SM, KIM JH, Choi JE, Noh KW, Kim IH. A Prospective, Long-term Follow up Study of 1444nm Nd:YAG Laser: A New Modality for the Treatment of Axillary Bromhidrosis and Hyperhidrosis. ASDS. 2010.10.
-To be continued-
▶ Next Artlcle : #10-1. Approach to Melanonychia