▶ Previous Artlcle : #11-1. Dermal Fibroblasts
Collagen is produced from various cells including the epithelial cells and smooth muscle cells, but the collagen involved in the tensile strength of wound is produced from dermal fibroblasts. Fibroblasts originate from special stem cells found in the adventitia of small blood vessels and take star, oblong or various other shapes. These fibroblasts around blood vessels appear at the wound three days after damage and migrate into the wound through the fibrous reticulum. This process continues until other fibroblasts accumulate and surround them. In other words, this migration is driven by chemotaxis. Undifferentiated mesenchymal cells migrating to the wound from adjacent healthy tissues differentiate into fibroblasts by the action of cytokines released from inflammatory cells, etc. Fibroblasts that have arrived earlier or have already differentiated stimulate migration of other fibroblasts.
[Advertisement] A-One LITE(Facial Diagnosys System) – Manufacturer: BOMTECH(www.bomtech.net)
Intercellular substances that play an important role in fibroblast adhesion and migration are fibrin, vitronectin, and fibronectin. When one pole of fibroblasts is anchored to fibronectin by integrin, the lamellipodia at the other pole travel toward fibronectic surface with the most appropriate receptor. Fibroblasts move along the fibril at the margin of the wound. This movement of fibroblasts is accelerated with rich hyaluronic acid of intercellular substances. Substances that attract fibroblasts to the wound are PDGF, TGF-β, EGF, lymphokine, collagen peptide and fibronectin, etc. Among these, TGF-β is an important factor that activates the release of proteolytic enzyme that helps fibroblast migration and promotes proliferation of fibroblasts.
Fibrolasts abound in the wound by the fifth day and dominate by the seventh day. Fibroblasts stop migration and synthesize collagen as their main function is switched to collagen generation 5-6 days after damage. The period where collagen synthesis has not yet begun is called lag phase. During this time, fibroblasts produce proteoglycan that serve as the ground substance for connective tissues to create an ideal biochemical environment for collagen generation and organization. Collagen generation is possible when the rough endoplasmic reticulum and Golgi apparatus abound within cells due to change in the nature of fibroblasts.
Now we will take a look at the clinical application of fibroblasts that synthesize collagen for tensile strength during wound healing.
Efforts to apply the dermal cells fibroblasts have continued to be made a long time ago. One method is the direct use of fibroblasts cultured in the culture plate. However, as the dermis mainly consists of ground substances including collagen and it is more important to replenish the dermal ground substance rather than cells themselves, various types of artificial dermis derived from fibroblasts were applied to treatment of chronic deep wound, rather than the direct use of fibroblasts. Also, attempts to use fibroblasts in gene therapy were made as it is easier to culture fibroblasts than other skin cells. There was a successful case of transplanting cultured autologous fibroblasts to recalcitrant diabetic leg ulcer.
In a report, autologous dermal fibroblasts were cultured for six weeks and injected in facial wrinkles and depressed scars three times with 2-3 week intervals and brought successful improvement. In another report, autologous dermal fibroblasts were cultured and combined with hyaluronic acid filler (Restylane). This was used in nasal dorsal augmentation and a 1-year follow-up revealed only 20-30% reduction and maintenance of effect.
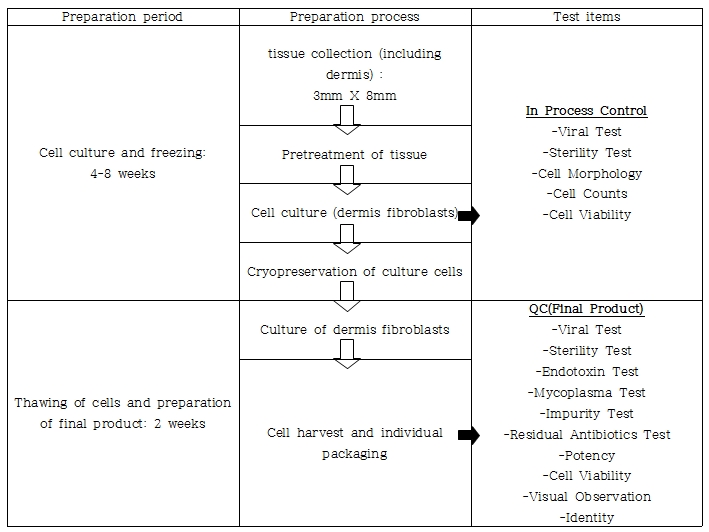
In particular, S.Biomedics, a cell-based therapy developer, earned the approval of Ministry of Food and Drug Safety of Korea for Cureskin, injectable autologous fibroblasts for scar treatment in 2010. Fibroblasts are collected from a patient’s skin sample, isolated and cultured up to a billion cells. Transplantation of cultured autologous fibroblasts into the dermis can generate collagen and other skin components from increased activated fibroblasts and brings wrinkle reduction and anti-aging effect. Therefore, cultured autologous fibroblasts therapy creates an environment similar to the youthful skin by stimulating self-renewal of existing fibroblasts and their differentiation into more mature skin cells. An innovative, new biomedical product using this technic for anti-aging procedures or skin regeneration in scar treatment has been developed.
However, this therapy involving culture and transplantation of autologous fibroblasts lacks prospective clinical data with long-term follow-up, despite the potential for wide indications, promising theoretical and preclinical outcome. An extensive follow-up study is needed to confirm the efficacy of this costly treatment. Although the actual injection is quick, it takes 4-6 weeks for tissue collection, culture and transplantation, not to mention the 2-3 month wait to see the effect. Efforts for shortening the process as well as patient education are needed.
References
❶ Eça LP, Pinto DG, de Pinho AM, Mazzetti MP, Odo ME. Autologous fibroblasts culture in the repair of aging skin. Dermatol Surg. 2012 Feb;38(2):180-4. ❷ Han SK, Shin SH, Kang HJ, Kim WK. Augmentation rhinoplasty using injectable tissue-engineered soft tissue: a pilot study. Ann Plast Surg. 2006 Mar;56(3):251-5. ❸ Boss WK Jr, Usal H, Chernoff G, Keller GS, Lask GP, Fodor PB. Autologous cultured fibroblastss as cellular therapy in plastic surgery. Clin Plast Surg. 2000 Oct;27(4):613-26. ❹ Watson D, Keller GS, Lacombe V, Fodor PB, Rawnsley J, Lask GP. Autologous fibroblastss for treatment of facial rhytids and dermal depressions. A pilot study. Arch Facial Plast Surg. 1999 Jul-Sep;1(3):165-70.
-To be continued-
▶ Next Artlcle : #12-1. Tissue Repair Stimulating Agent with Nucleic Acid