Conservative and Surgical Treatemtns of Vascular Lesions
Due to the high possibility of spontaneous regression, hemangioma is seldom treated in the early phase; however, early aggressive treatment may be required when the lesion grows abruptly, covers important sites, such as the eye, nose, mouth or anus, or is accompanied by hemorrhage or platelet reduction. Intralesional steroid (Kenalog) of low dose (3-5mg/kg) is injected every 6-8 weeks for small lesion, or oral steroid (prednisolone) is prescribed (2-3mg/kg/day) for large and abruptly growing hemangioma. Steroids should be limited to severe cases only, because they may induce side effects, such as immunodeficiency, hormone disorders or bone growth disorders. Interferon (ITF 2a/2b, 2-3 mil unit/m2) or chemotherapy (vincristine, CP, bleomycin) may be considered for patients not responding to steroids.
Hemangioma is surgically managed when it accompanies hemorrhage or ulcer, or covers the eyelid or important areas. Since surgery may leave a scar, care should be taken when deciding whether or not to perform a surgery if the hemangioma is expected to be regressed. Hemangiomas seldom return to normal skin even after spontaneous regression and require plastic surgery for the vestige or scar left in more than 50% of patients.
[Advertisement] ▶ Aileen plus(Long pulsed Nd:YAG Laser) – Manufacturer: FineMEC(www.finemec.net)
Facial superficial capillary malformation (PWS) does not require a surgery but is manageable by laser therapy. However, laser therapy will not be sufficient, and even a surgery may not be available, for deep and extensive mixture of capillary malformation, lymph node malformation and venous malformation. Facial vascular malformation is distributed widely across the normal facial tissues, and surgical removal may result in damaging normal tissues, such as facial skin, muscle and nerve; therefore, it is difficult to make a decision whether or not to perform a surgery, and even there is a limitation in surgical removal.
Facial sclerotherapy with ethanol or thrombojet injection under fluoroscopy or embolization can be performed to obstruct the blood vessel. Local sclerotherapy can be used as well by percutaneous injection.
Since the face is distributed by various blood vessels supplied from a number of places, embolization rarely results in complete cure, but is often used as a preoperational adjuvant therapy to reduce blood flow.
Facial sclerotherapy should be performed carefully by experienced intervention radiologists, because it may move along the blood flow and infiltrate into the cerebral vessels and may even cause severe side effects, including blindness when it infiltrates into the eye.
Therapeutic effect of laser therapy by vascular disease
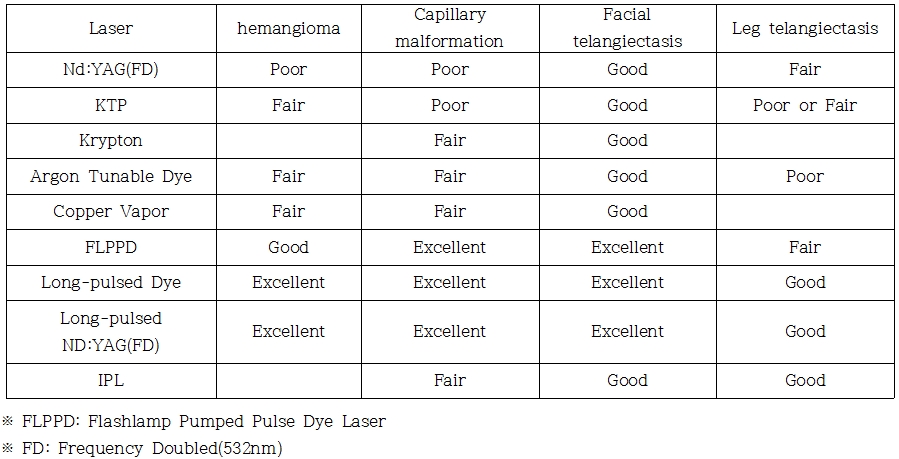
Laser Treatment of Vascular Lesions
The most important aspect in laser treatment of vascular lesions is the wavelength. Hemoglobin the main chromophore of skin with maximum absorption at 412nm and 577nm, but 585-595nm is used due to shallow penetration depth. Deeper 2-3mm penetration requires 800-1064nm wavelength.
The size of capillary is 10-50μm and grows thicker to 300μm with age. Laser pulse duration depends on the size of blood vessel, but has to be shorter than capillary thermal relaxation time (TRT); 20-500μsec is used depending on the size of blood vessel. As for fluence, 4.5J/cm2 or higher is used so as to inflict thermal injury to endothelium. Higher output may damage the surrounding tissues.
As for the diameter of laser beam, 5mm, 7mm or 10mm tip is commonly used. Larger diameter delivers better efficacy, when the energy output is the same, but smaller diameter should be used when using higher output.
Pulsed dye laser of 575nm was developed targeting hemoglobin of vascular lesions. Because it had less than 1mm penetration depth, however, 585nm flash lamp pumped pulse dye laser was developed later for penetration to 1.2mm. Afterward, in order to overcome the limitations of FLPPD, 590-595nm lasers with higher output was developed for penetration deeper in the dermis and preservation of the epidermis with coolant.
VersaPulse® laser was an effective, water cooled system, but later has become a representative case where the product had to die out of the market after the company (Coherent) was merged by another company (Lumenis), leaving a lot of products out of the reach of customer service in Korean market.
Vbeam with long 595nm wavelength provides cooling effect of the epidermis by spraying the coolant and the high output allows superior therapeutic effect than the former FLPPD.
IPL has not one but multiple (500-1200nm) wavelengths, which can be irradiated selectively on skin. When absorbed in hemoglobin in the skin, it is effective for telangiectasis and small blood vessels of 1-2mm or less in diameter. Pulse duration is 2-25msec, and output is 3-30J/cm2, which is less effective than lasers developed specifically for vascular therapy.
As pulsed dye laser with longer wavelength is also limited in the treatment of vascular lesions deeper than the dermis, 1064nm Nd:YAG laser can be used for such lesions. The non-selective tissue damage may leave sequela, including scar and decoloration.
Nd:YAG laser can be used with fiber optic guide as an interstitial laser for deep facial lesions, although it is associated with the risk of causing facial palsy or injury to the facial expression muscles. When carefully used per sites, this can be beneficial for deep vascular lesions that have no alternatives.

Figure 5. Facial and cervical superficial capillary malformation (PWS) markedly improved by 2 courses of Vbeam laser therapy.

Figure 6. Hemangioma on an infant’s forehead completely removed by 595nm laser therapy.
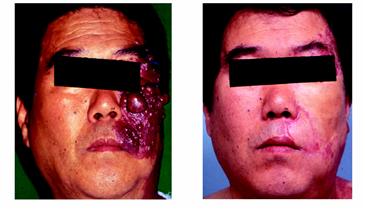
Figure 7. Vascular malformation becomes raised and the blood vessels thickened with age, precluding laser therapy and sometimes requiring surgical resection and skin transplantation.
Vascular malformation thinly distributed across the skin responds well to laser therapy, but not the vascular malformation under the subcutaneous fat layer. Skin vascular malformation with perforator vessel from below can also respond to laser therapy, although the malformation is recurrent.
I have also felt the limitations of vascular malformation treatments. After visiting the Vascular Anomaly Center at Boston Children’s Hospital, the leading hospital in vascular malformation around the globe, and Dr. Mulliken’s clinic, who has great enthusiasm for research and classification of vascular malformation, I learned the importance of team approach for vascular malformation. They held conference on vascular malformation every week and had discussions about various cases among the team members. They also provided multidisciplinary approach, including surgical resection, embolization, sclerotherapy and medical management, as well as laser therapy. In addition to basic research on vascular malformation, a laser that can selectively treat deeper lesions is needed.
Reference: Laser Plastic Surgery, Koonja Publishing, 2008, Seoul
- The End -
▶ Previous Artlcle : #6. Laser Treatment for Hemangioma and Vascular Malformation Ⅰ