▶ Previous Artlcle : #9-2. Surgical Treatment of Axillary Hyperhidrosis
Case
Patient: 54-year-old female
Chief complaint: Thickened toenails with increased black stripes (Figure 1, Period: >6 years).
Past history and family history: Not remarkable.
Skin and physical findings: Not remarkable.
[Advertisement] MAGNUM(Q-switched Nd:YAG Laser) – Manufacturer: (www.i-dana.com)]
Examination findings: No particular abnormality was detected in a recent physical examination.
Diagnosis: Onychomycosis was diagnosed based on the fungus detection in KOH test. Dermoscopy (Figure 1) confirmed that matrix histology was not necessary. Onychomycosis and secondary melanonychia were diagnosed.
Treatment: The patient could be completely recovered by using oral and topical (for nails) antifungal agents.
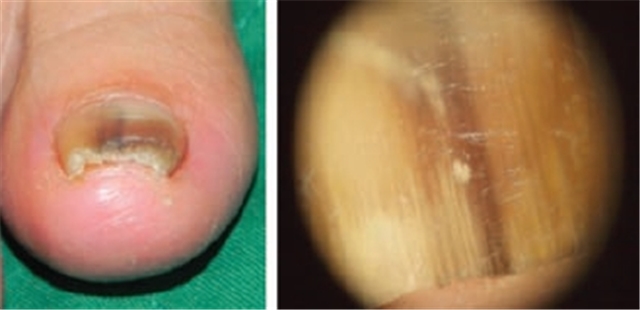
Figure 1. Onychomycosis accompanying melanonychia
Approach to the Diagnosis of Melanonychia
I. Nail avulsion
1. Conventional avulsion
1) Indications
- To confirm lesions at the bottom of nails, nail matrices, and inside the proximal and lateral nail folds
- To prepare for histology or matricectomy
- To relieve symptoms of dysplastic or hyperplastic nail plates
- Adjuvant therapy for reducing the period of systemic antifungal therapy for onychomycosis
2) Contraindication – No absolute contraindication.
3) Limitations – Avulsed hand nails grow back in 6 months, during which time the elaborate workmanship may be reduced. Toenails grow back in 1 year and the soft tissue at the end of the toe may be elevated, causing some discomfort with ‘round up’ walking. Previous pathology can develop again as new nails grow. Nail dysplasia may become permanent after nail matrix histology.
2. Patient should be informed of the following issues before the surgery:
1) Indications and the process of the procedure
2) Discontinuation of anticoagulants or other drugs that may affect the blood coagulation
3) Dressing: The use of hands may be limited and slippers are needed for feet because lesions will be covered widely with gauze.
4) Dressing may be replaced on a daily basis and there may be a slight pain and discharge.
5) Limitation of activities: Daily activities may be limited after removing toenails.
6) The nail bed can become thick or hard until a new nail grows back again (pseudo-nail).

Figure 2. Partial nail dysplasia may still continue after matricectomy for longitudinal melanonychia.
3. Preparations for surgery
1) Preoperative evaluations:
Medical history – Bleeding tendency; Infection – hepatitis, HIV, etc.; Transplantations such as artificial heart valve; Allergies; Peripheral vascular diseases; and Peripheral nerve disorders
Physical examination: Nail plate examinations
Local anesthesia and sterilization.
Devices required for the surgery: Freer septum elevator, dental spatula, or blunt hemostat, Iris scissors, Skin hooks or fine-toothed forceps, electrocautery, double action nail clippers (bone rongeur), nail splitting scissors, English nail splitter, scalpel blade No. 11 and No. 15, disposable punch (2,3,4,5,6 mm), tourniquet (Penrose drains), Leur-Lock syringe, 30-gauge needle and Prolene 6-0.

Figure 3. Partial nail avulsion and matricectomy
4. Postoperative management
1) Pain control – Oral acetaminophen or acetaminophen containing codeine
2) Dressing: Change on a daily basis. Apply antibiotic ointment, and cover the lesion with Gelform for hemostasis, several layers of gauze, and elastic bandage.
5. Possible complications: Continuous hemorrhage, persistent or severe pain, permanent nail destruction or loss.
-To be continued-
▶ Next Artlcle : #10-2. Approach to Melanonychiac