▶ Previous Artlcle : #10-1. Approach to Melanonychia
II. Matrix histology
1. Indications: Discoloration of nail plates, detection of lump, unexplained change in nail unit
2. Contraindication: No absolute contraindication.
3. Limitations: Basically similar to those of nail avulsion. Permanent onycholysis or longitudinal ridging may occur after the histology.
4. Patient should be informed of the following issues before the surgery:
1) Indications and outcomes expected when the histology is not conducted.
2) Process of the procedure
3) The possibility of permanent dysplasia, especially after matrix histology
4) The possibility of the need for suture and revisit for its removal
5) The possibility of limitation in activities
5. Postoperative management: Same as the pain control, dressing and possible complications described for nail avulsion.
[Advertisement] DEPILIGHT(808 Diode laser for Hair Removal) – Manufacturer: DANIL SMC(www.danilsmc.com)
Discussion on the approach to the diagnosis of melanonychia
When the color of a nail is partially or completely turned brown or black, nail avulsion and matrix histology are conducted to find the cause. It is called ‘melanonychia’ when increased melanocytes are the cause, or ‘longitudinal melanonychia’ when the lesion appears in vertical lines (Figure 3). Because melanonychias are manifested in a variety of forms, it is difficult to differentiate them only with the naked eye. Therefore, nail avulsion followed by histology are often necessary for differential diagnosis (Figure 4-5).

Figure 4. Longitudinal melanonychia-nevus
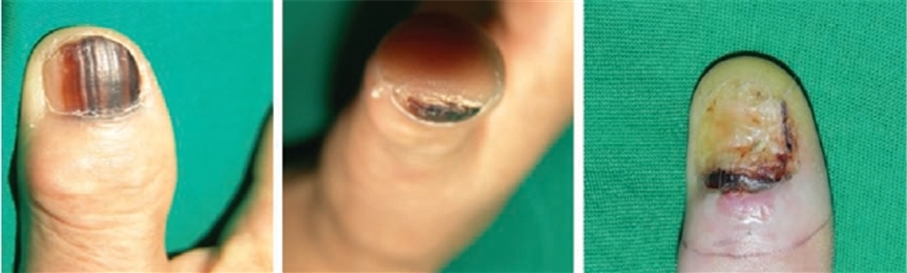
Figure 5. Melanonychia with positive Hutchinson’s sign where the blackness has spread to the cuticle. Melanoma in situ was diagnosed by histopathological examination.
Differential diagnoses requiring histology include lentigo simplex, melanocytic nevus, drug side effects, fungal infection and malignant melanoma. Unlike in adults, longitudinal melanonychia in infants is mostly benign, requiring observation of prognosis for several months to see if the lesion is naturally disappeared and how the color changes before conducting histology. Longitudinal melanonychia accompanied by mottled hyperpigmentation on the lips and oral mucosa is Laugier-Hunziker syndrome, a disease of unknown cause occurring mostly in white female. Antitumor agents can be a cause of melanonychia, and most of the cases involve more than two nail plates and accompanies transverse melanonychia as well, allowing differentiation from early malignant melanoma. The causative bacteria of melanonychia by fungal infection include Scopulariopsis brevicaulis, Trichophyton rubrum, and Scytalidium dimidiatum. Histology of nail matrix should be considered in the following cases for differentiation from malignant melanoma: 1. adults with melanonychia, particularly with the thumbnail or big toenail becoming gradually wider or darker; 2. children with nail plate pigmentation becoming wider or darker; and 3. patients who are suspected of longitudinal melanonychia by Bowen’s disease beneath the nail plates or subungual keratosis. When pigmentation widens slightly, Hutchinson’s sign is not accurately detectable with the naked eye. Dermoscopy before nail avulsion can be very useful for clinical diagnosis and differential diagnosis for malignancy in this case, because it can confirm irregular line thickness, widening and spreading to cuticle quite accurately on brown background (see references below for details). Before conducting a nail surgery, such as nail avulsion, general examinations should be performed to eliminate peripheral vascular diseases, diabetes mellitus, hematologic disorders, connective tissue diseases, peripheral nerve diseases, artificial heart valve, poor hygiene and immunosuppression, as well as an investigation on concomitant medications (e.g., MAO inhibitors, beta-blockers, phenothiazine, anticoagulants including aspirin, systemic or topical steroids, retinoids). Local anesthesia is contraindicated for patients with hypersensitivity to lidocaine or paraben and those with heart disease.
Before conducting histology or surgery, infection should be detected based on the texture and color of the skin surrounding the nail lesion compared to normal skin on the other side, if any, treated with proper antibiotics. Simple X-ray, ultrasonography or MRI can be used for bone or soft tissue imaging. The lesion should be swabbed with or soaked in povidone-iodine. There are various methods of local injection for anesthesia; but for anesthesia of the whole finger or toe, the best option is ring block technique, which gives anesthetic to both lateral sides along the nerve. Lidocaine 1% or 2% is most commonly used for anesthesia. Epinephrine may enhances the visibility of surgical site with its vasoconstriction effect, but it is advised to avoid because of the risk of peripheral tissue necrosis. Instead, tourniquet can be used, desirably for less than 1 hour. A fine injection needle (25-30 gauges) is inserted perpendicularly to both lateral sides at the base of finger where nerve passes through. After touching the periosteum, the needle is pulled back and 1 ml local anesthetic is injected. The needle is tilted 45 degrees toward the palmar direction and then dorsal direction and 1 ml is injected, respectively. The same process is repeated for the opposite side. It takes about 5-10 minutes for the anesthetic effect to kick off. When testing or removing discoloration, nevus or small tumor on nail matrix, they should be removed by shaving if they are suspected as benign. Transverse, rather than longitudinal, incision in nail matrix should be adopted to minimize nail malformation. Longitudinal incision may create tension, possibly causing nail ridges or nail splitting.
References
1. Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27: 580~584.
2. Tosti A, Piraccini BM, de Farias DC. Dealing with melanonychia. Semin Cutan Med Surg 2009; 28: 49~54.
3. Koga H, Saida T, Uhara H. J Dermatol. Key point in dermoscopic differentiation between early nail apparatus melanoma and benign longitudinal melanonychia. 2011 Jan;38(1):45~2.
-To be continued-
▶ Next Artlcle : #11-1. Treatment approaches for Basal Cell Carcinoma of Face in Koreans and Mohs Micrographic Surgery